Ethics and Public Health
Selected resources from The Hastings Center.
Bioethics Briefings:
Public health encompasses what society does to assure the conditions that are necessary for its members to be healthy, including economic, social, and environmental factors. The public health tradition adopts a preventative orientation and views health from the population-level, guided by a commitment to social justice. Read our briefing to consider the question: What are the potential trade-offs and synergies between collective goods and individual interests in healthcare?
From Hastings Bioethics Forum:
- How Bioethicists Can Respond to the Moment by Learning from the PastHistory is informative in considering how bioethicists should respond to serious new threats to public health and well-being.
- Bioethics Must Address War as a Public Health CrisisToday’s wars kill far more civilians than soldiers. Bioethics must address war not just as an individual tragedy but as a public health disaster.
- New York City’s Involuntary Commitment Plan: Fulfilling a Moral Obligation?After a string of violent crimes involving mentally ill people who are homeless, New York City Mayor Eric Adams announced a plan for police and emergency medical workers to involuntarily remove people with severe mental illness from the streets and bring them to hospitals for psychiatric evaluation. Mayor Adams said we have a “moral obligation” to help people who are mentally ill. But is this plan moral?
- Should Ethicists Be at the Table in Public Health Policy Deliberations?In a recent article in The New England Journal of Medicine, Ezekiel Emanuel and colleagues clearly illustrate the relevance of ethical considerations to policy deliberations concerning public health emergencies. But do ethicists belong at the table?
- Philanthropy is Not Enough: Oil and Gas Giants Must Consider Medical EthicsGiven the well-known environmental and health risks of oil and gas drilling, oil and gas giants that enter developing nations routinely offset these risks with charitable investments. Are these investments sufficient? Do the funds go where they are needed? Answering this question raises ethical issues that need greater attention.
- Public Health Officials and Gun Rights Advocates Must Work TogetherIn rural Virginia, where I live, there is strong support for the right to own and carry guns. For more than a decade, I have shared public health, mental health, and other scientific findings with the leadership of a statewide Second Amendment rights advocacy group, especially regarding the leading number of deaths by firearms: suicide. We do not agree on what firearms laws and policies might be or do to prevent suicides, but we have sustained our conversations and respectfully learned from each other’s point of view. Such conversations are hard to have.
- Treating Gun Violence as a Public Health Threat: Not Exactly What We MeantThis week, the United States saw two momentous public health events: one million deaths attributed to Covid and the 198th mass shooting of the year. Both the pandemic and gun shootings are threats to public health that are not being adequately addressed.
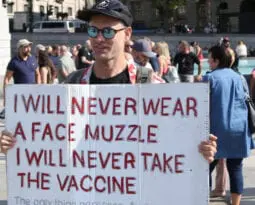
- Rugged American Individualism is a Myth, and It’s Killing UsThe American myth of rugged individualism, which often means “pulling yourself up by your own bootstraps,” is outdated, was never completely accurate. It is on full display during the coronavirus pandemic, contributing to cases and deaths.
- C.D.C.’s Latest Mask Guidance: Science, Politics, and Public HealthThe C.D.C.’s latest policy guidance that people who have been fully vaccinated against the coronavirus virus no longer need to wear face masks indoors gets the science right, but policymaking wrong.
- Bruce Springsteen: The Latest Celebrity DWIIt was especially disappointing to read about Bruce Springsteen’s recent arrest for suspicion of driving while intoxicated (DWI). Here’s hoping the famous rocker will use his arrest to refocus attention on a risky and dangerous behavior that is thoroughly preventable.
- Science in the Biden White House: Eric Lander, Alondra Nelson, and the Legacy of Lewis ThomasScience has replaced populism in the White House. For the first time, the president’s science advisor will be elevated to cabinet rank. There are other good omens, as well.
- Motivated Ignorance: A Challenge for Science Communication and DemocracyMany people are deeply interested in the political process and awash in relevant information., but nevertheless often grossly misinformed, holding confident but unfounded opinions at odds with widely accessible evidence The recent riot at Capitol Hill is just one illustration–albeit a horrifying one–of such misinformation and its potential consequences. The anti-vaccine movement is another example.
- Resisting Public Health Measures, Then and NowOne of the most surprising aspects of the Covid-19 pandemic for those of us who teach the history of public health is how unwilling many Americans have been to adopt health measures to protect others. Over the Thanksgiving holiday, tens of millions of Americans traveled, despite the fact that the Centers for Disease Control and Prevention urged them to stay home and the overall death rate from the coronavirus is approaching 300,000. Should recent events make us revisit aspects of the history of public health? And how can these stories inform future public health efforts during pandemics?
- Are Physicians Hypocrites for Supporting Black Lives Matter Protests and Opposing Anti-Lockdown Protests? An Ethical AnalysisPhysicians have been vocal in condemning the anti-lockdown protests while endorsing and even participating in the Black Lives Matter protests. This has led to criticism of the medical community for being inconsistent and hypocritical. What does an ethical analysis reveal?
- Lawsuits of Last Resort: Employees Fight for Safe Workplaces during Covid-19As more workplaces open up, a seldom-used legal action is being taken against employers charged with inadequately protecting employees from the coronavirus: public nuisance lawsuits.
- Pandemic Language
- Social-Change Games Can Help Us Understand the Public Health Choices We FaceBefore there was the Covid-19 pandemic, there was Pandemic. This tabletop game, in which players collaborate to fight disease outbreaks, debuted in 2007. Expansions feature weaponized pathogens, historic pandemics, zoonotic diseases, and vaccine development races. Game mechanics modelled on pandemic vectors provide multiple narratives: battle, quest, detection, discovery. There is satisfaction in playing “against” disease–and winning. Real pandemic is not as tidy as a game. But can games support understanding about the societal challenges we now face? Yes.
- After the Surge: Prioritizing the Backlog of Delayed Hospital ProceduresThe rewards of social distancing are beginning to accrue in former hotspots such as Seattle, the New York metropolitan area, and the San Francisco Bay Area, where the number of new Covid-19 cases requiring hospitalization is declining. Assuming the rewards hold in the face of pressures to reopen the economy, hospitals will now face challenges of reopening their own nonpandemic services for patients whose elective surgeries and other procedures were postponed. Which patients should get priority?
- Individual Freedom or Public Health? A False Choice in the Covid EraWhen scientists first suggested population-wide social distancing as the only feasible way to suppress Covid-19, they were the first to admit it may not work in a free society. We are now months into placing mass restrictions on human behavior to suppress a virus that lacks an effective vaccine or treatment. Now is the time to ask: is this the authoritarian nightmare many feared, or will freedom and democracy survive Covid-19?
- Beyond the Covid Crisis—A New Social Contract with Public HealthCovid-19 is teaching us the stern lesson that economic well-being and health justice are two sides of the same coin. To weather pandemics and restore the social contact that economic life demands, we need to sign a new social contract with public health.
- Show Me Your Passport: Ethical Concerns About Covid-19 Antibody Testing as Key to Reopening Public LifeAround the world, governments are looking for safe ways to lift unprecedented restrictions on public activities to curb the spread of Covid-19. So-called immunity passports could be key to the effort to selectively ease restrictions for people presumed to be immune to the virus. But there are scientific and ethical questions to be worked out before they can be deployed. .
- Ethics and Evidence in the Search for a Vaccine and Treatments for Covid-19In the rush to find a Covid-19 vaccine and one or more drugs to treat the deadly disease, concerns are being raised that ethical standards for conducting human clinical trials and the evidentiary standards for determining whether interventions are safe and effective, might be loosened.
- U.S. and Canada: Being Good Neighbors in the PandemicCanada has a fraction of the number of cases of Covid-19 as the U.S. Canadians feel vulnerable. But Canadians and Americans need to find ways to build and maintain trust within and across our borders.
- The Price of Going Back to Work Too Soon
- We Need International Medical Graduates to Help Fight Covid-19. Immigration Policies Keep Them Away
- Coronavirus Response Is Insufficient for Vulnerable New Yorkers
- Health Care for Obesity and Eating Disorders: What Needs to ChangeThe theme of National Eating Disorder Awareness (NEDA) week , “Come as you are: Hindsight is 20-20,” is designed to encourage those recovering from eating disorders to reflect on their journeys towards body acceptance. It also affords doctors and other health professionals an opportunity to evaluate how well they are doing to help patients reach this goal.
- Report from China: Ethical Questions on the Response to the CoronavirusHastings Center fellows in China discuss ethical questions about the response to the spreading coronavirus.
- The Public Charge Rule Is a Eugenic Policy
- From Outcry to Solidarity with Migrants: What Is the Good We Can Do?Another June. Another public outcry about cruelty as policy harming migrants in United States custody. This summer, the photo of a drowned family, Óscar Alberto Martínez Ramírez and his daughter, Valeria, of El Salvador, shocks the conscience. Reporters are documenting the inhumane conditions in a Border Patrol facility where hundreds of children have been held. How should our field respond?
- Forced from Home: Evicting Immigrants from Public Housing Harms Children’s HealthThe federal government’s proposed rule to disqualify families from public housing if any member is undocumented will harm children, families, and cities.
- Staying in Their Lane: Health Professionals Must Address Gun ViolenceIn the wake of the recent Twitter fight between the National Rifle Association and U.S. physician groups over whether doctors should speak out about firearm policy issues, we argue that professionalism actually requires that doctors take a leadership role in gun…
- Immigrant Health and the Moral Scandal of the “Public Charge” RuleA long-anticipated policy change proposed by the Trump administration that would count the use of many federally-subsidized programs against immigrants currently eligible to use them threatens public health and would undermine ethical practice in health professions and systems. The policy would…
- Newspaper Op-Eds Should Disclose Authors’ Industry TiesEarlier this month, The Seattle Times published an op-ed by Samuel Browd, medical director of Seattle Children’s Sport Concussion Program, on the risks of brain injury in youth sports. Dr. Browd acknowledged troubling research on the dangers of repetitive brain trauma, but…
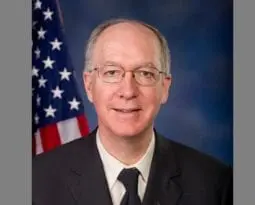
- The Only PhD Scientist in Congress Speaks About Truth, Politics, and Human FlourishingAt a time when facts are distorted, disregarded, and ignored in policy making and political discourse, the need in Washington for seekers and defenders of truth has perhaps never been greater. I discussed the state of affairs with Representative Bill Foster,…
- Is it Time to Regulate the Sale of Sugar to Minors?In “Tackling Obesity and Disease: The Culprit Is Sugar; the Response is Legal Regulation,” published in the Hastings Center Report, Lawrence O. Gostin describes four coordinated interventions that have been effective at controlling peoples’ tobacco consumption and which can serve as…
- After Hurricane Harvey, Injustice in HoustonHurricane Harvey dissipated in September, but much of the destruction that it wreaked on Texas and Louisiana remains. When addressing residential concerns, disaster relief officials prioritize the newly homeless over the chronically homeless, choosing to protect the previously privileged over the…
- After the Election Bioethics Faces a Rocky RoadAcademic bioethics has never been popular with Republicans. Libertarians dislike academic bioethics because it seems too elitist and anti-free market. Religious thinkers worry it is technocratic, soulless and crassly utilitarian. Now with Trumpism add a populist disdain for expertise, experts and…
- Lincoln’s Promise: Congress, Veterans, and Traumatic Brain InjuryPerhaps we were naïve. Our plan was relatively simple: we would chart the legislative evolution of programs for veterans with traumatic brain injuries (TBI) to identify policy gaps for this underserved and vulnerable population. With recent media attention highlighting the U.S….
- The Good of the BodyThe December 2015 United Nations meeting on climate change was an historic moment for global efforts to reduce harmful carbon emissions. While it gained the agreement about the future good of the planet, it made clear that there is a long…
- Responding to Zika: Ethical Challenges of Zoonotic DiseasesThe World Health Organization will hold an emergency committee meeting on the pandemic reemergence of Zika virus and the explosive increase in reported cases of congenital microcephaly in Brazil possibly linked to Zika on February 1. The virus is a mosquito-borne infection in…
- Responding to Ebola: Health Care Professionals’ Obligations to Provide CareAs health care institutions in the United States prepare for Ebola patients, many have adopted the policy that those providing hands-on care should come from a pool of volunteers. Given the mixed history of health care providers’ willingness to care for patients during…
- How Bioethicists Can Help Reduce Global Health InequitiesThe state of global health is a major concern. Despite advances in medicine and medical care and massive growth of the global economy, health in the world is characterized by widening disparities within and between countries; lack of access to even…
- Belief in a Just World: A Case Study in Public Health EthicsWhy did portraying a married, working, loving, family-oriented, and religious couple with a disabled child bring out consistently negative reactions among the public toward allowing this family access to government-subsidized health care for their children? The answer may lie in a…
From Hastings Center Report:
Examining the Ethics and Impacts of Laws Restricting Transgender Youth-Athlete Participation
First published: 07 June 2023
Abstract
As of this writing, twenty-one states have passed laws barring transgender youth-athletes from competing on public-school sports teams in accordance with their gender identity. Proponents of these regulations claim that transgender females in particular have inherent physiological advantages that threaten a “level playing field” for their cisgender competitors. Existing evidence is limited but does not support these restrictions. Gathering more robust data will require allowing transgender youth to compete (rather than preemptively barring them), but even if trans females are shown to retain some advantage, this would not have greater moral significance than the many other “fair” physical and economic advantages found across sports. These regulations deprive transgender youth, an exceptionally vulnerable population, from the vast physical, mental, and social benefits of sports. While we advocate for transgender inclusion under our current, gender-segregated model of sport, we propose changes to the overarching structure that would promote a more inclusive and fairer athletic environment.
Public Health at the Kitchen Table: Lessons from the Home HIV Test’s Long Road to Approval
First published: 24 February 2023
Abstract
Home diagnostic testing is becoming part of the modern medical landscape, but many ethical and policy questions remain unresolved. Most of them first surfaced during the long regulatory deliberations over the home HIV test, the first home test for a contagious illness sold in the United States. Between 1989 and 2012, federal regulators and their consultants debated the ideal metrics for such a test, its benefits, and its potential harms for both individuals and communities. Ultimately, two iterations of the home HIV test were marketed in the United States; neither one of them changed the course of the national HIV epidemic, as hoped. This failure has powerful implications for home testing for other contagious diseases.
Expanding Paid Sick Leave Laws: The Public Health Imperative
First published: 24 February 2023
Abstract
A key public health measure has received far too little attention over the course of the Covid-19 pandemic: paid sick leave policies that encourage people at risk of spreading disease to stay home rather than come to work. The United States is one of the only developed countries that fails to guarantee paid sick leave at the federal level, leaving a patchwork of state and private policies that undersupply time off when people are contagious and protect top wage earners at wildly disproportionate rates compared with what workers with lower incomes experience. Other countries have shown that sick leave mandates are neither unjustified burdens on employers nor gratuitous giveaways to employees. In fact, sick leave saves on health care costs by making employees less likely to infect coworkers, to be absent for longer themselves, or to need treatment in expensive hospital emergency departments. Nationally guaranteed sick leave is urgently needed to promote public health.
Louisiana’s “Medically Futile” Unborn Child List: Ethical Lessons at the Post-Dobbs Intersection of Reproductive and Disability Justice
First published: 06 January 2023
Abstract
Ableist attitudes and structures are increasingly recognized across all sectors of health care delivery. After Dobbs, novel questions arose in the United States concerning how to protect reproductive autonomy while avoiding discrimination against and devaluation of disabled persons. In this essay, we examine the Louisiana Department of Health’s emergency declaration, “List of Conditions That Shall Deem an Unborn Child ‘Medically Futile,’” issued August 1, 2022. We raise a number of medical, ethical, and public health concerns that lead us to argue that the declaration should be rescinded. Analysis of this ethically objectionable declaration provides valuable lessons about how to uphold both reproductive and disability justice in a post-Dobbs landscape.
Protecting Health after Dobbs
First published: 20 December 2022
Abstract
In Dobbs v. Jackson Women’s Health Organization, the Supreme Court eliminated the long-standing federal constitutional right to abortion. Discussions ofDobbs tend to emphasize the loss of protection for reproductive choice. But Dobbs also eroded protection for a related yet distinctly important interest that served under Roe v. Wade as a check on government regulation of reproduction: the preservation of health. This erasure has opened the door to increasingly restrictive and punitive abortion bans, which are causing providers to deny or delay care that is necessary to prevent harm to both pregnant and nonpregnant patients. Federal regulatory attempts to prevent these harms will have limited impact, partially due to Congress’s own history of exceptionalizing abortion in ways that devalue health. Only federal legislation can ensure adequate and enduring protection for the health of women, trans men, and other patients targeted for reproductive control because of their capacity for pregnancy.
An Ecostructural Lens for Health Ethics
First published: 20 December 2022
Abstract
In this commentary, I describe an ecostructural approach to health ethics, which is grounded in a conception of people as ecological subjects and privileges place in supporting health and health justice. This approach sees people as dwelling in health ecosystems that can support or undermine health, and it situates us in social norms and processes, with a particular concern for structural health injustice. In patient care, an ecostructural approach can be operationalized by attending to conditions in the sites where birthing, healing, and dying take place and by critiquing their economic structures. For public health, relationships between people, animals, land, the built environment, and climate demand attention, as do racist norms and economic processes that thwart health justice. For global health, an ecostructural approach might envision a revolution in governance that challenges nationalism, in which health systems treat citizens while depending on human resources supplied through structures that sustain health injustice.
Zoonoses and Animal Culling: The Need for One Health Policy
First published: 13 October 2022
Abstract
One Health (OH) as a biomedical and social movement calls to reorient public health approaches toward more holistic, nonanthropocentric approaches that do not exclude the interests of animals and ecosystems. OH thus urges reexamination, from both scientific and moral perspectives, of the practice of culling pet, farm, or wild animals in the face of a zoonosis. Pandemics such as Covid and monkeypox highlight the need for more rigorous analysis of the justifications traditionally provided to back these culling practices. Such analyses should then ground reasonable OH policies and legislation that consider the rights of humans, animals, and the environment. Bill S.861, “Advancing Emergency Preparedness through One Health Act of 2021,” which was introduced in the U.S. Congress, is a step in the right direction.
Bioethics in Community Health
First published: 22 August 2022
Abstract
What keeps community health providers up at night? And how should bioethics evolve to meet the needs of these providers? Hastings Center research scholar Nancy Berlinger introduces a new project and line of research and public-facing work at The Hastings Center to explore ethical challenges that arise in primary and preventative health care for medically underserved communities, where ethical challenges often reflect the health consequences of social inequalities.
Covid-19: Medical Decisions, Mandates, and High-Risk Minors
First published: 28 June 2022
Abstract
Kensey Dishman was unvaccinated when she contracted Covid-19 at thirteen years old. She also had asthma and is now dead. Her divorced parents disagreed about whether Kensey should be vaccinated, and her father suggested that it was Kensey’s own choice to refuse vaccination. This situation is as complicated as it is tragic, and it raises a number of legal and ethical issues regarding medical decision-making for minors, parental rights, vaccination mandates, and individual freedom versus government interests in protecting minors as well as public health. This commentary explores these issues and highlights potential sources of liability for those involved in Kensey’s treatment decisions given her high-risk for complications from Covid-19.
Racism, Not Race: A Physician Perspective on Anti-Black Racism in America
First published: 26 April 2022
In this commentary, which responds to the article “Anti-Black Racism as a Chronic Condition,” by Nneka Sederstrom and Tamika Lasege, I draw on my experience as a physician who cares for a largely Black patient population. Physicians are trained to “first do no harm” and strive to treat patients to the best of their abilities. However well intentioned, many of us fall short of this goal and witness the consequences of health inequities that disproportionally impact the lives of Black patients. Recent years have brought increased acknowledgment and understanding of social determinants of health, but these modest changes fail to identify the true culprit of health disparities. Racism, not race, is responsible for the negative outcomes that we see in our communities of color. Both subtle and overt forms of systemic racism plague the educational systems and scientific metrics of medicine in the United States. Physicians’ training, culture, and biases are founded in White norms. To decenter Whiteness as a normality, medicine must enact a multipronged approach that begins with increasing the diversity of physicians and providers to better reflect the patients that they care for. Bioethicists must publicly state that racism is real and that we are dedicated to changing it, but to get beyond statements, we must also have a measure of improvement and success in battling racism.
Now You Are Part of the Solution: Bioethicists’ Contribution in Addressing Racialized Health Inequity
First published: 26 April 2022
Abstract
Neoliberalism (an economic approach emphasizing tax abatement, market deregulation, and social safety net reduction) promotes inequality and unfavorable health outcomes. These outcomes are exacerbated among racial and ethnic minorities, as this policy approach is often coupled with various forms of institutional racism. The combination of these factors translates into concerning population health disparities in the United States. More egalitarian policies could disproportionately affect the socially marginalized and help rectify these challenges. Given the social and cultural capital bioethicists have in the fields of medicine, public health, and policy, this group is uniquely positioned to help remediate racial and ethnic inequity. Moreover, the unique skill sets bioethicists employ (conflict resolution, mediation, negotiation, facilitating public engagement, policy analysis) can be useful to improving the health of the populous. Thus, bioethicists can play a key role in addressing the most concerning health challenges and inequities today.
Anti-Black Racism and Power: Centering Black Scholars to Achieve Health Equity
First published: 26 April 2022
Abstract
In health equity research, anti-Black racism and power imbalances manifest at every phase of the research process and contribute to the marginalization and exclusion of Black scholars. This essay highlights how power operates as a central component of anti-Black racism, and I describe the importance of centering Black scholars in funding, conducting, and implementing health equity research. Interdisciplinary collaboration between the fields of bioethics, public health ethics, and health equity could generate dialogue and develop recommendations to help balance power dynamics, address anti-Black racism, and, ultimately, make meaningful progress toward health equity.
Holding Them Accountable: Organizational Commitments to Ending Systemic Anti-Black Racism in Medicine and Public Health
First published: 26 April 2022
Abstract
In this essay, I detail commitments that some of the major health organizations—the American Medical Association, the American Public Health Association, and the Centers for Disease Control and Prevention—have made to addressing anti-Black racism and discuss their policies meant to curtail racism’s effects on health equity. Although these organizations’ historical lack of action has contributed to a culture of anti-Black racism in health care and public health and many Black people have suffered because of it, progress has to begin somewhere, and outlining their future actions is a good start. Now, bioethicists, with our expertise in how historic policies connect to contemporary disparate health outcomes and access to health care, are in a position to hold these organizations accountable for fulfilling their commitments.
A Call for Solidarity in Bioethics: Confronting Anti-Black Racism Together
First published: 26 April 2022
Abstract
In this short piece, an Indigenous, community-based public health researcher who supported the development of this special report describes this collection as a call for all bioethicists to work together for justice, and she highlights the importance of listening to the truths spoken in this report and of amplifying its messages.
Allocation of Opportunities to Participate in Clinical Trials during the Covid-19 Pandemic and Other Public Health Emergencies
First published: 15 December 2021
Abstract
Covid-19 raised many novel ethical issues including regarding the allocation of opportunities to participate in clinical trials during a public health emergency. In this article, we explore how hospitals that have a scarcity of trial opportunities, either overall or in a specific trial, can equitably allocate those opportunities in the context of an urgent medical need with limited therapeutic interventions. We assess the three main approaches to allocating trial opportunities discussed in the literature: patient choice, physician referral, and randomization/lottery. As, we argue, none of the three typical approaches are ethically ideal for allocating trial opportunities in the pandemic context, many hospitals have instead implemented hybrid solutions. We offer practical guidance to support those continuing to face these challenges, and we analyze options for the future.
Restructuring Deliberation Using a Cultural Theory Lens
First published: 14 December 2021
Abstract
Designing broad public deliberation is challenging. In addition, participants of public deliberation are guided by their cultural norms, values, and rules. This creates a tension between the goal of practical approaches to broad public deliberation and how individuals perceive issues and relate to others in the world. Despite such challenges, we must continue to create opportunities for the public to deliberate about and provide input into the regulation of emerging technologies. Therefore, previously imagined approaches to broad public deliberation should be reevaluated to better utilize the information gained during the process and expand the range of ideas incorporated into decision-making. To do this, institutions must consider how the public makes sense of complex issues concerning cultural conflict. This article introduces a framework that demonstrates how cultural theory can be used for rethinking previous approaches to public deliberation. In doing so, it offers guidelines for designing public deliberation involving distinct public participation venues based on different worldviews.
Justice, Bioethics, and Covid-19
First published: 14 December 2021
Abstract
Both articles in the November-December 2021 issue of the Hastings Center Report reflect bioethics’ growing interest in questions of justice, or more generally, questions of how collective interests constrain individual interests. Hugh Desmond argues that human enhancement should be reconsidered in light of developments in the field of human evolution. Contemporary understandings in this area lead, he argues, to a new way of thinking about the ethics of enhancement—an approach that replaces personal autonomy with group benefit as the primary criterion for deciding what enhancements are acceptable. In the second article, Johannes Kniess considers the many attempts within bioethics to draw on John Rawls’s work to discuss health care access and social determinants of health, and he comes across as moderately optimistic that Rawls’s theory of justice has ongoing relevance.
Covid-19, Free Exercise, and the Changing Constitution
First published: 16 November 2021
Abstract
The Covid-19 pandemic has brought bioethics back to five topics—justice, autonomy, expert authority, religion, and judicial decisions—that were central during its formative period but has cast a new light on each, while also tangling public health policy in the current, rather radical, reshaping of the role of organized religion in society.
Covid Vaccine Mandates and Religious Accommodation in Employment
First published: 08 November 2021
Abstract
Many employers are requiring their employees to be vaccinated for Covid-19 to comply with federal, state, or local laws, or to conform to employers’ policies. Some employees object to vaccination on religious grounds. Title VII of the Civil Rights Act of 1964 prohibits discrimination in employment based on religion and requires employers to reasonably accommodate employees’ religious beliefs or practices unless doing so would be an undue hardship to the employer’s business. Although a religion need not be an established faith with many followers, philosophical or political objections do not count as religious beliefs. If an employee demonstrates a bona fide religious objection, the issue is whether it can be reasonably accommodated. This will depend on the employer’s business, including whether close contact with coworkers or customers is required.
Pediatric Off-Label Use of Covid-19 Vaccines: Ethical and Legal Considerations
First published: 08 November 2021
Abstract
When the U.S. Food and Drug Administration fully approved the Pfizer-BioNTech Covid-19 vaccine for people sixteen and older, questions arose. Parents, pediatricians, and the media wondered whether Covid-19 vaccines could be used off-label—and whether they should be. The American Academy of Pediatrics cautioned against pediatric off-label use of the vaccine, and the vaccine provider agreement from the Centers for Disease Control and Prevention appears to prohibit it. After briefly contextualizing ethical and legal precedents regarding off-label use, we offer an analysis of the ethical permissibility of and considerations for pediatric off-label Covid-19 vaccination based on individual benefits, risks, and available alternatives. Our analysis challenges the ethics of a blanket prohibition on off-label pediatric Covid-19 vaccination, as it limits clinician ability to provide care they may determine to be clinically and ethically appropriate. At the same time, our analysis acknowledges that Covid-19 creates population-level ethical considerations that are at times in tension with individual health interests.
Material Insecurity, Racial Capitalism, and Public Health
First published: 13 September 2021
Abstract
In the influential 1995 article “Social Conditions as Fundamental Causes of Disease,” Bruce Link and Jo Phelan described social and political factors as “fundamental causes” of death and disease. Whitney Pirtle has recently declared racial capitalism another such fundamental cause. Using the case of the water crisis in Flint, Michigan, she has argued that racial capitalism’s role in that situation meets each of the criteria Link and Phelan’s article outlines: racial capitalism influenced multiple disease outcomes, affected disease outcomes through multiple risk factors, involved access to flexible resources that can be used to minimize both risks and the consequences of disease, and was reproduced over time through the continual replacement of intervening mechanisms. We argue for Pirtle’s conclusion using the extensive literature on racial capitalism and case studies concerning housing in the United States and Brazil and what Naomi Klein has termed “corona capitalism” in India. If races correspond to hierarchies of material security, as suggested by Ruth Wilson Gilmore, then these hierarchies and their causal effects are fundamental determinants of public health.
Opioid Treatment Agreements and Patient Accountability
First published: 13 July 2021
Abstract
Opioid treatment agreements are written agreements between physicians and patients enumerating the risks associated with opioid medications along with the requirements that patients must meet to receive these medications on an ongoing basis. The choice to use such agreements goes beyond the standard informed consent process and has a distinctive symbolic significance. Specifically, it suggests that physicians regard it as important to hold their patients accountable for adhering to various protocols regarding the use of their opioid medications. After laying out a taxonomy of accountability relations between physicians and patients, I argue that opioid treatment agreements are justifiable for physicians to use in their provision of care only if they improve patient or public health outcomes, which has yet to be demonstrated.
What Has Covid-19 Exposed in Bioethics? Four Myths
First published: 24 May 2021
Abstract
The Covid-19 pandemic has exposed four myths in bioethics. First, the flood of bioethics publications on how to allocate scarce resources in crisis conditions has assumed authorities would declare the onset of crisis standards of care, yet few have done so. This leaves guidelines in limbo and patients unprotected. Second, the pandemic’s realities have exploded traditional boundaries between clinical, research, and public health ethics, requiring bioethics to face the interdigitation of learning, doing, and allocating. Third, without empirical research, the success or failure of ethics guidelines remains unknown, demonstrating that crafting ethics guidance is only the start. And fourth, the pandemic’s glaring health inequities require new commitment to learn from communities facing extraordinary challenges. Without that new learning, bioethics methods cannot succeed. The pandemic is a wake-up call, and bioethics must rise to the challenge.
Antiracist Praxis in Public Health: A Call for Ethical Reflections
First published: 11 April 2021
Abstract
The Covid-19 pandemic has revealed myriad social, economic, and health inequities that disproportionately burden populations that have been made medically or socially vulnerable. Inspired by state and local governments that declared racism a public health crisis or emergency, the Anti-Racism in Public Health Act of 2020 reflects a shifting paradigm in which racism is considered a social determinant of health. Indeed, health inequities fundamentally rooted in structural racism have been exacerbated by the Covid-19 pandemic, which calls for the integration of antiracist praxis to promote ethical public health research processes. This commentary describes ways in which antiracist praxis—which emphasizes empowerment of traditionally marginalized populations—offers strategies to explicitly address power imbalance, stigmatization, and other consequences of structural racism in public health research.
Does a Public Health Crisis Justify More Research with Incarcerated People?
First published: 23 March 2021
Abstract
Covid-19 has infected thousands and killed hundreds in prisons, jails, and immigration detention facilities across the United States. Responding to this crisis, leading medical researchers have called for expanding opportunities for people in prison to participate in vaccine trials. These calls, like current regulations, focus on individualized risk assessments around consent, coercion, and harm, while ignoring the unnaturalness of deprivation conditions in U.S. prisons. We need new frameworks of analysis that refocus on structural, rather than individual, risk assessments. Integrating structural perspectives—including skepticism of claims of scarcity, avoidance of representational distortions, and attention to institutional agency—into our existing, overly individualistic frameworks might permit the design of more ethical research projects involving people who are incarcerated. Still, the unnatural deprivations of incarceration might be so great that research subjects might need to be removed from prison entirely in order to ethically participate in research.
Creative Democracy—the Task Still before Us
First published: 25 February 2021
Abstract
This essay looks to Thomas Jefferson and John Dewey, as well as a contemporary political theorist, Kevin O’Leary, for some guidance in confronting the present crisis in American democratic norms and practices—including that swirling around issues of public health.
Civic Learning, Science, and Structural Racism
First published: 25 February 2021
Abstract
Vaccine hesitancy is a major public health challenge, and racial disparities in the acceptance of vaccines is a particular concern. In this essay, we draw on interviews with mothers of Black male adolescents to offer insights into the reasons for the low rate of vaccination against the human papillomavirus among this group of adolescents. Based on these conversations, we argue that increasing the acceptance of HPV and other vaccines cannot be accomplished merely by providing people with more facts. Instead, we must address the pervasive racial discrimination in the United States that undermines trust in social institutions, including the health care system. In the short term, it may be helpful to increase the number of clinicians of color working in the health system, but more fundamental changes are required. The U.S. must adopt and implement policies that dismantle structural racism if it hopes to produce greater trust and community-oriented thinking on behalf of people who have been exploited for centuries.
Restricting Reasons: A New Battleground in Abortion Regulation
First published: 23 October 2020
Abstract
The latest trend in abortion restrictions in the United States targets a woman’s reasons for terminating a pregnancy. Fourteen states have attempted to enact laws prohibiting abortion on the basis of fetal sex, race, and/or genetic anomaly. These laws are different from regulations tied to a government interest in protecting women’s health. Laws that restrict reasons implicate a different set of government interests to be weighed against a woman’s constitutional right first recognized inRoe v. Wade. These laws also seek to reframe the nature of the right asserted by the woman. To date, the Supreme Court has declined to address the constitutionality of laws that restrict reasons, and the Court’s most recent abortion decisions provide little guidance.
It is possible that a conservative majority of the Supreme Court would uphold a law that prohibits reasons for having an abortion that appear discriminatory. But such laws would be difficult to enforce and therefore may be relegated to policy statements rejecting discriminatory norms as opposed to being effective means of restricting access to abortion.
A Futile Use of Futility
First published: 28 August 2020
Abstract
As the rates of intravenous opioid use have increased, so have its associated medical complications, such as endocarditis, and known interventions, such as heart-valve replacements. For many patients, including Jacob, whose case was brought to my psychiatric consult service and to my colleagues in the clinical ethics service, relapse increases the risk of repeat endocarditis and the need for repeat surgical interventions. Previous works have posed the bioethical quandary regarding the responsibilities of a surgeon in these repeat procedures and whether a surgeon may ethically refuse to perform a repeat intervention in a patient who has relapsed. Notions of futility are commonly used to navigate this complex terrain, and they were the focus of the ethics consideration given to Jacob’s case, in which surgeons were reluctant to perform valve replacements. In this narrative essay, I interrogate the concept of futility by appealing to its history and variable meanings, and I argue against its relevance in cases like Jacob’s. I propose that a more suitable bioethical approach in such cases would consider resource allocation, the sociocultural stigma of addiction, and the interpersonal and narrative factors that make each case unique.
Solving the Opioid Crisis Isn’t Just a Public Health Challenge—It’s a Bioethics Challenge
First published: 28 August 2020
Abstract
Among those who discuss America’s opioid crisis, it is popular to claim that we know what we, as a society, ought to do to solve the problem—we simply don’t want it badly enough. We don’t lack knowledge; we lack the will to act and to fund the right policies. In fact, I’ve heard two versions of this. Among those who focus on prescription opioids, it is clear that we ought to stop prescribing so many powerful opioid painkillers. And among my public health colleagues focusing on illicit drug use, it is clear that we ought to expand addiction treatment and harm-reduction services. The problem, however, is that the second claim is not obvious (and, indeed, is denied by many Americans), and the first claim probably isn’t even true (at least, not in so crude a form). In short, the opioid crisis presents not only a problem of political will but also one of ethics. It will take work to discover or justify our normative claims in this arena.
Toward Fair and Humane Pain Policy
First published: 28 August 2020
Abstract
Pain policy is not drug policy. If society wants to improve the lives of people in pain and compress the terrible inequalities in its diagnosis and treatment, we have to tailor policy to the root causes driving our problems in treating pain humanely and equitably. In the United States, we do not. Instead, we have proceeded to conflate drug policy with pain policy, relying on arguably magical thinking for the conclusion that by addressing the drug overdose crisis, we are simultaneously addressing the pain crisis. This is a category error, decades of commitment to which have resulted mostly in a worsening of both public health problems. Disentangling our problems in treating pain fairly and equitably from our problems with drugs and substance use is the only path to humane and ethical policy for each.
Rethinking the Importance of the Individual within a Community of Data
First published: 07 July 2020
Abstract
The Covid-19 crisis has underscored the importance of the collection and analysis of clinical and research data and specimens for ongoing work. The federal government recently completed a related revision of the human subjects research regulations, founded in the traditional principles of research ethics, but in this commentary, we argue that the analysis underpinning this revision overemphasized the importance of informed consent, given the low risks of secondary research. Governing the interests of a community is different from governing the interests of individuals, and here we suggest that, moving forward, the analyses of the risks of secondary research protocols be assessed from the perspective of the former.
62,406 and Counting
First published: 29 June 2020
Abstract
What will we remember, as scholars, practitioners, policy-makers, educators, and citizens, about this acute phase of the catastrophe in the United States? The shocking federal failure concerning testing? That the first shortage was not of ventilators but protective gear? How infection rates and deaths in communities of color, immigrant neighborhoods, and nursing homes mercilessly exposed the relationship between social inequalities and health inequities? I hope we will remember that the field of bioethics did good work under pressure, learned that public health ethics and global health ethics are about securing the conditions for decent lives and decent work as well as saving lives, and committed ourselves to progress on the problem of inequality.
AI Surveillance during Pandemics: Ethical Implementation Imperatives
First published: 29 June 2020
Abstract
Artificial intelligence surveillance can be used to diagnose individual cases, track the spread of Covid-19, and help provide care. The use of AI for surveillance purposes (such as detecting new Covid-19 cases and gathering data from healthy and ill individuals) in a pandemic raises multiple concerns ranging from privacy to discrimination to access to care. Luckily, there exist several frameworks that can help guide stakeholders, especially physicians but also AI developers and public health officials, as they navigate these treacherous shoals. While these frameworks were not explicitly designed for AI surveillance during a pandemic, they can be adapted to help address concerns regarding privacy, human rights, and due process and equality. In a time where the rapid implementation of all tools available is critical to ending a pandemic, physicians, public health officials, and technology companies should understand the criteria for the ethical implementation of AI surveillance.
Digital Contact Tracing, Privacy, and Public Health
First published: 29 June 2020
Abstract
Digital contact tracing, in combination with widespread testing, has been a focal point for many plans to “reopen” economies while containing the spread of Covid-19. Most digital contact tracing projects in the United States and Europe have prioritized privacy protections in the form of local storage of data on smartphones and the deidentification of information. However, in the prioritization of privacy in this narrow form, there is not sufficient attention given to weighing ethical trade-offs within the context of a public health pandemic or to the need to evaluate safety and effectiveness of software-based technology applied to public health.
Interdependent Citizens: The Ethics of Care in Pandemic Recovery
First published: 29 June 2020
Abstract
The crisis of Covid-19 has forced us to notice two things: our human interdependence and American society’s tolerance for what Nancy Krieger has called “inequalities embodied in health inequities,” reflected in data on Covid-19 mortality and geographies. Care is integral to our recovery from this catastrophe and to the development of sustainable public health policies and practices that promote societal resilience and reduce the vulnerabilities of our citizens. Drawing on the insights of Joan Tronto and Eva Feder Kittay, we argue that the ethics of care offers a critical alternative to utilitarian and deontological approaches and provides a street-ready framework for integration into public health deliberations to anchor public policy and investments concerning the recovery and future well-being of America’s citizens and society.
Older Adults and Covid-19: The Most Vulnerable, the Hardest Hit
First published: 29 June 2020
Abstract
Older adults in the United States have been the age group hardest hit by the Covid pandemic. They have suffered a disproportionate number of deaths; Covid patients eighty years or older on ventilators had fatality rates higher than 90 percent. How could we have better protected older adults? Both the popular press and government entities blamed nursing homes, labeling them “snake pits” and imposing harsh fines and arduous new regulations. We argue that this approach is unlikely to improve protections for older adults. Rather than focusing exclusively on acute and critical resources, including ventilators, a plan that respected the best interests of older adults would have also supported nursing homes, a critical part of the health care system. Better access to protective equipment for staff members, early testing of staff members and patients, and enhanced means of communication with families were what was needed. These preventive measures would have offered greater benefit to the oldest members of our population than the exclusive focus on acute care.
Vulnerable Children in a Dual Epidemic
First published: 29 June 2020
Abstract
Two epidemics—Covid-19 and opioid use disorder (OUD) —are creating short- and long-term mental and physical health risks for vulnerable children and adolescents. Information about the risks to children from exposure to the coronavirus is still fragmentary, but even many healthy children are not getting appropriate health care, such as vaccinations or monitoring of developmental milestones during the Covid-19 pandemic. Children living in poverty are at heightened risk. Youngsters who are already dealing with OUD in their families—2.2 million as of 2017—face serious consequences stemming from trauma and stress. Although not officially designated by the Centers for Disease Control and Prevention as “adverse childhood experiences” (“ACEs”), these situations meet the CDC’s criteria for inclusion, such as death or separation from a parent. It is important to recognize and meet the needs of all these children now and not just when the long-term consequences become apparent.
Scarcity in the Covid-19 Pandemic
First published: 20 April 2020
Abstract
As we write, U.S. cities and states with extensive community transmission of Covid-19 are in harm’s way—not only because of the disease itself but also because of prior and current failures to act. During the 2009 influenza pandemic, public health agencies and hospitals developed but never adequately implemented preparedness plans. Focused on efficiency in a competitive market, health systems had few incentives to maintain stockpiles of essential medical equipment. Just-in-time economic models resulted in storage of only those supplies needed then. At the same time, global purchasing in search of lower prices reduced the number of U.S. suppliers, with hospitals dependent on foreign companies. There is still a possibility that the pandemic will be manageably bad rather than unmanageably catastrophic in this country. Immediate, powerful, and sustained federal action could make the difference.
Responding to Covid-19: How to Navigate a Public Health Emergency Legally and Ethically
First published: 26 March 2020
Abstract
Few novel or emerging infectious diseases have posed such vital ethical challenges so quickly and dramatically as the novel coronavirus SARS-CoV-2. The World Health Organization declared a public health emergency of international concern and recently classified Covid-19 as a worldwide pandemic. As of this writing, the epidemic has not yet peaked in the United States, but community transmission is widespread. President Trump declared a national emergency as fifty governors declared state emergencies. In the coming weeks, hospitals will become overrun, stretched to their capacities. When the health system becomes stretched beyond capacity, how can we ethically allocate scarce health goods and services? How can we ensure that marginalized populations can access the care they need? What ethical duties do we owe to vulnerable people separated from their families and communities? And how do we ethically and legally balance public health with civil liberties?
Pediatric Drug Labeling and Imperfect Information
First published: 18 February 2020
Abstract
I first became aware of bioethics in the spring of 1980. I had spent a thirty-six-hour shift shadowing a medical resident, and I was struck that many of the resident’s decisions had ethical dimensions. The next day, I came across the Hastings Center Report, and I realized I wanted to explore ethical issues I found implicit in clinical care, even though I still wanted to become a pediatrician. In September 2019, when I attended my first meeting of the U.S. Food and Drug Administration’s Pediatric Advisory Committee, as a pediatric pulmonologist, I had the same sense of awe and curiosity that I had forty years ago. What had appeared initially as somewhat technical decisions about the regulation of drug labeling was suffused with ethical questions. The committee was asked to discuss possible changes to the labeling of two previously approved drugs.
Trust in American Medicine: A Call to Action for Health Care Professionals
First published: 18 February 2020
Abstract
Medical mistrust has a well-documented harmful impact on a range of patients’ health behaviors and outcomes. It can have such egregious downstream effects on so many aspects of medicine—from clinical trial participation to health care use, timely screening, organ donation, and treatment adherence—that it is sometimes described as one of the social determinants of health. In the article “Trust, Risk, and Race in American Medicine,” Laura Specker Sullivan makes the compelling case that trust is essential to building a therapeutic alliance in which effective, high-quality health care can be delivered and received. As a complement to her suggestion that health care providers take an active role in mitigating mistrust by demonstrating “not only their capacity to be honest and forthright but also their ability to respond to the potential truster’s needs,” we recommend that key health care professionals commit to five actions.
Sugar, Taxes, & Choice
First published: 08 December 2019
Abstract
Population obesity and associated morbidities pose significant public health and economic burdens in the United Kingdom, United States, and globally. As a response, public health initiatives often seek to change individuals’ unhealthy behavior, with the dual aims of improving their health and conserving health care resources. One such initiative—taxes on sugar-sweetened beverages—has sparked considerable ethical debate. Prominent in the debate are arguments seeking to demonstrate the supposed impermissibility of SSB taxes and similar policies on the grounds that they interfere with individuals’ freedom and autonomy. Commentators have often assumed that a policy intended to restrict or change private individuals’ consumption behavior will necessarily curtail freedom and, as a corollary, will undermine individuals’ autonomy with respect to their consumption choices. Yet this assumption involves a conceptual mistake. To address the misunderstanding, it’s necessary to attend to the differences between negative liberty, freedom of options, and autonomy. Ultimately, concerns about negative liberty, freedom, and autonomy do not provide strong grounds for opposing SSB taxes.
Asylum, Refuge, and Justice in Health
First published: 03 July 2019
Abstract
We are, as of May 2019, witnessing yet another “caravan” of people fleeing violence in Latin America, bonding together to reach the territory of safer states in the North. Similarly, in the fall of 2015, Europe experienced the movement of many refugees fleeing war, persecution, and grave human rights violations in Syria. These new waves of people on the move have raised anew important questions about asylum and refuge: who should be able to claim asylum? Should the fear of persecution be sufficient, or do asylum seekers need to show that they have actually suffered it? And maybe most controversially, how should asylum-granting states respond to the plight of those asking for asylum on their territory?
The moral principles guiding asylum and refuge are different from the rules usually regulating immigration, which are based on the principle of territorial sovereignty that allows nation-states to discriminate and select among those who hope to immigrate. Asylum and refuge instead call upon nation-states to provide refugees with a new home, protect human rights, and over time, provide access to the social, political and civic rights that characterize membership. Included in the list of human rights, I will argue, is the provision of the means for individual physical and psychological well-being.
Controlling Measles through Politics and Policy
First published: 22 April 2019
Abstract
Vaccination is one of history’s most successful public health interventions. Since 2000, vaccination campaigns against measles, which is highly contagious but preventable through the measles-mumps-rubella (MMR) vaccine, have reduced both the global incidence of the disease and measles deaths by 80 percent. However, progress toward measles elimination has slid backward in several previously well-protected global regions. With more communities below or at risk of falling below the 95 percent immunization rates required for herd immunity—due more and more to vaccine skepticism and declination rather than lack of access—many U.S. states and countries must reappraise their vaccination policies and programs.
Conscience and Religious Freedom Division Marks Its First Anniversary with Action
First published: 18 April 2019
Abstract
In January 2018, the Trump administration established the Conscience and Religious Freedom Division within the Department of Health and Human Services’ Office of Civil Rights with the explicit goal of intensifying legal protection of religious and conscience objections in health care. The establishment of OCR’s new division illustrates the significant powers of administrative agencies to mold the substance of law without seeking legislative action. The mere formation of a division dedicated to protecting conscience rights is already having a significant impact; it is causing health care entities, including hospitals, research organizations, and clinics, to change policies and practices to comply with the declared enforcement strategy. Administrative agencies also shape the law in what they decide not to pursue. For example, OCR has suspended enforcement of the Affordable Care Act prohibition against gender-identity discrimination.
Federal Right to Try: Where Is It Going?
First published: 18 April 2019
Abstract
Policy-makers, bioethicists, and patient advocates have been engaged in a fierce battle about the merits and potential harms of a federal right-to-try law. This debate about access to investigational medical products has raised profound questions about the limits of patient autonomy, appropriate government regulation, medical paternalism, and political rhetoric. For example, do patients have a right to access investigational therapies, as the right-to-try movement asserts? What is government’s proper role in regulating and facilitating access to drugs that are still in development? In this review, we analyze the history of the right-to-try movement, review the arguments put forth by supporters and opponents of the legislation, and consider the movement’s consequences. Two possible scenarios may emerge. One is that the right-to-try pathway may fail to meaningfully increase patient access to investigational products. Alternatively, certain companies may attempt to rely on the federal right-to-try legislation to sell investigational products, taking advantage of the provision that allows for direct costs, as there is currently no clear mechanism for enforcement or monitoring of cost calculations.
The Critical Role of Medical Institutions in Expanding Access to Investigational Interventions
First published: 18 April 2019
Abstract
The U.S. federal government provides two tracks for eligible patients to obtain access outside clinical trials to investigational interventions currently under study for potential clinical benefits: the Food and Drug Administration’s expanded access pathway and the pathway created by the more recent Right to Try Act. In this issue of the Hastings Center Report, with a critical focus on patients, industry, and the research enterprise, Kelly Folkers and colleagues frame the inherent challenges that these pathways are meant to solve and have also inadvertently created. But an additional key focus is how the relevant situations should be managed at the bedside and how the system risks both inefficient and inequitable access to options at the institutional level. Although either pathway could be helpful to patients, the challenges of having the pathways coexist are greater than the sum of their parts. Individual clinicians represent the front line of the regulatory and eligibility challenges of expanded access and right to try, making clinical education a critical component of a comprehensive approach to using them well. But it is medical institutions that must take the lead on supporting access to investigational options in the most equitable and effective manner possible.
Citizen Science and Gamification
First published: 18 April 2019
Abstract
According to the mainstream conception of research involving human participants, researchers have been trained scientists acting within institutions and have been the individuals doing the studying, while participants, who are nonscientist members of the public, have been the individuals being studied. The relationship between the public and scientists is evolving, however, giving rise to several new concepts, including crowdsourcing and citizen science. In addition, the practice of gamification has been applied to research protocols. The role of gamified, crowdsourced citizen scientist is new in the domain of scientific research and does not fit into the existing taxonomy of researchers and participants. We delineate and explicate this role and show that, while traditional roles are governed by well-established norms and regulations, individuals engaged in gamified, crowdsourced citizen science—gamers—fall through the cracks of research protections and regulations. We consider the issues this raises, including exploitation and the absence of responsibility and accountability. Finally, we offer suggestions for how the current lack of appropriate norms may be rectified.
Social Media, E-Health, and Medical Ethics
First published: 21 February 2019
Abstract
Given the profound influence of social media and emerging evidence of its effects on human behavior and health, bioethicists have an important role to play in the development of professional standards of conduct for health professionals using social media and in the design of online systems themselves. In short, social media is a bioethics issue that has serious implications for medical practice, research, and public health. Here, we inventory several ethical issues across four areas at the intersection of social media and health: the impact of social networking sites on the doctor-patient relationship, the development of e-health platforms to deliver care, the use of online data and algorithms to inform health research, and the broader public health consequences of widespread social media use. In doing so, we review discussions of these topics and emphasize the need for bioethics to focus more deeply on the ways online technology platforms are designed and implemented. We argue that bioethicists should turn their attention to the ways in which consumer engagement, bias, and profit maximization shape online content and, consequently, human behavior and health. We also offer a set of recommendations and suggest future directions for addressing ethical challenges in these domains.
Ethical Use of Social Media Data: Beyond the Clinical Context
First published: 21 February 2019
Abstract
In “Social Media, e-Health, and Medical Ethics,” in this issue of the Hastings Center Report, Mélanie Terrasse, Moti Gorin, and Dominic Sisti address and suggest recommendations for several ethical issues central to the systematic ethical analysis of the effects of social media on clinical practice, health services research, and public health. The topic is as timely as it is important: social media data collected by device and web applications are constantly increasing and might have both individual and public health benefits. The authors focus their analysis primarily on the health care context. Yet the implications of the intersection of social media data and research warrant focused consideration, as even the most thorough ethical analysis in the clinical context is not necessarily directly applicable in the research context. While many ethical issues are present in both settings, the research context poses new challenges and calls for consideration of distinct factors. In particular, because the legal framework is less protective in research, critical ethical analysis of the research-specific issues and considerations is essential to the ethical conduct of research using social media data as well as to the design and operation of social media device and web applications themselves.
Taking a Systems Approach to Chronic Illness in Old Age
First published: 11 October 2018
Abstract
We are living through a demographic transition from a world in which there were lots of young people and very few older adults to one in which the numbers in these age groups are becoming more evenly balanced. One reason for this is that more of us are living into our seventies, eighties, nineties, and beyond. That is the good news. Unfortunately, the chance of developing chronic illnesses (including diabetes, arthritis, and dementia) is typically higher for people in these older age groups than for those who are younger. Because we do not know how to cure these illnesses, many of us will spend at least some of this extra time with one or more chronic illness. While we are more likely than in the past to live into older age, we are likely to be living with illness when we get there. That raises a challenge: how should we respond to this change?
Housing, the Built Environment, and the Good Life
First published: 11 October 2018
Abstract
At any age, the pursuit of a good life is easier in a physical environment that promotes health, supports activities important to self-fulfillment, and facilitates connections to the larger community. In old age, the home and neighborhood environments are particularly important: they are the locations where older people spend most their time, and they can have a great impact on independence, social connection, feelings of self-worth, and physical and emotional well-being.
Within the urban planning field, home and neighborhood characteristics are important dimensions of debates about the measurement of human progress and quality of life, particularly as an alternative to purely economic measures. They are also key issues in public health, particularly as they relate to physical, social, and mental well-being. Here, we focus on how to improve the fit of environments for people as they age.
Proposed Regulations Favor Providers’ Conscience Rights over Patients’ Rights
First published: 16 August 2018
Abstract
In establishing a new Conscience and Religious Freedom Division within the Office of Civil Rights of the Department of Health and Human Services and issuing new proposed regulations, the Trump administration has significantly expanded the power of health care providers over the medical choices of patients and has privileged the moral agency of health care providers over that of individual patients. When finalized, these regulations will replace those promulgated during the Obama administration, just as those regulations replaced those promulgated in 2008 by the Bush administration. The 2018 proposed regulations interpret the federal conscience statutes more broadly than either of these predecessors. Among the many significant provisions in the proposed rules are definitional terms that reach a broader range of individuals and activities, the absence of balancing interests, and a powerful enforcement structure.
Defining Misprescribing to Inform Prescription Opioid Policy
First published: 16 August 2018
Abstract
Prescription opioid policies too often reflect over a century’s worth of moralizing about the nature of opioid use disorder, the value of pain, and the meaning of suffering. The social and legal penalties to prescribers run in one direction—avoid overprescribing, however defined, at all costs. The lack of shared definitions is problematic for formulating and evaluating opioid policy. For example, the variant definitions of “misuse,” “abuse,” and “addiction” complicate estimates of morbidity. There are also no widely accepted definitions of misprescribing and overprescribing. I offer here a modest attempt at the categorization of misprescribing: inadvertent overprescribing, corrupt overprescribing, qualitative overprescribing, quantitative overprescribing, multiclass overprescribing, and underprescribing.
Are Obese Children Abused Children?
First published: 16 August 2018
Abstract
In 2010, a South Carolina mother was taken to court when her fourteen-year-old son reached 555 pounds. An article on the story reported, “His mother, Jerri Gray, lost custody of her son and is being charged with criminal neglect. Gray is facing 15 years on two felony counts, the first U.S. felony case involving childhood obesity.” If the caretakers of obese children are negligent, then they are also morally and legally blameworthy. I want to suggest, however, that important ethical differences exist between negligent or abusive caretakers and the caretakers of obese children and that these differences ought to make a moral and legal difference. The distinctions are nuanced, and the ethical pictures in cases of abuse, neglect, and obesity are far from black and white. However, the various types of harm that children face from their caretakers should be placed in neither the same ethical nor the same legal category.
When children are beaten or sexually molested, the justification for taking them out of the home is clear: the caretakers are violating the rights of their children. Similarly, with neglect, caretakers are failing to provide their children the necessities to which they are entitled. The central question that I want to address in this article is whether the actions (or inaction) of caretakers that allow a child to become obese are morally or practically analogous to physical abuse or neglect. Ultimately, I will argue that parenting that allows a child to become obese is so morally different from both abuse and neglect that it is best understood as falling outside these categories altogether. This conclusion has important moral, practical, and legal implications.
What Genomic Sequencing Can Offer Universal Newborn Screening Programs
First published: 14 August 2018
Abstract
Massively parallel sequencing, also known as next-generation sequencing, has the potential to significantly improve newborn screening programs in the United States and around the world. Compared to genetic tests whose use is well established, sequencing allows for the analysis of large amounts of DNA, providing more comprehensive and rapid results at a lower cost. It is already being used in limited ways by some public health newborn screening laboratories in the United States and other countries—and it is under study for broader and more widespread use, including as a core part of newborn screening programs. Sequencing technology has the potential to significantly improve these essential public health programs. For many of the conditions that newborns are already screened for, sequencing can return more specific and more sensitive results. The technology could also enable newborn screening programs to expand the list of rare pediatric conditions that they look for, thereby identifying more infants who can benefit from immediate care.
A New Era, New Strategies: Education and Communication Strategies to Manage Greater Access to Genomic Information
First published: 14 August 2018
Abstract
As next-generation genomic sequencing, including whole-genome sequencing information, becomes more common in research, clinical, and public health contexts, there is a need for comprehensive communication strategies and education approaches to prepare patients and clinicians to manage this information and make informed decisions about its use, and nowhere is that imperative more pronounced than when genomic sequencing is applied to newborns. Unfortunately, in-person counseling is unlikely to be applicable or cost-effective when parents obtain genomic risk information directly via the Internet. As a rule, communication strategies should match how people are accessing health information. Today, many people can obtain health information in a variety of settings, including through direct-to-consumer services, via websites, and through other digital channels or settings. In response to these changes, new communication strategies need to be considered. Adopting a comprehensive communication model means understanding the multiple levels of influence experienced by parents and the clinicians who serve them. In addition, applying communication-science principles can help in addressing some key challenges to effectively communicating genomic information to parents.
Single-Gene Sequencing in Newborn Screening: Success, Challenge, Hope
First published: 14 August 2018
Abstract
Some state-based newborn screening programs in the United States already use sequencing technology, as a secondary screening test for individual conditions rather than as a broad screening tool. Newborn screening programs sequence an individual gene, such as the cystic fibrosis transmembrane conductance regulator, which causes cystic fibrosis, after an initial biochemical test suggests that a baby might have a condition related to that gene. The experiences of state public health departments with individual-gene sequencing illustrate both the usefulness of the technology and its complexities. Here I discuss how newborn screening programs investigate cystic fibrosis and, as another example, adrenoleukodystrophy through individual gene sequencing.
Mass Shootings, Mental Illness, and Gun Control
First published: 28 March 2018
Abstract
In the wake of the Stoneman Douglas School shooting, Republican and Democratic leaders—like the American electorate they represent—remain sharply divided in their responses to gun violence. They are united in their condemnation of these mass shootings, but they disagree about whether stricter or looser gun control laws are the answer. Those on the right side of the political aisle suggest that the issue is one of mental illness rather than gun control. Conversely, those who are more liberal or progressive in their political learnings are quick to condemn attempts to reframe the issue of mass shootings as a mental health problem. Both sides are wrong. Mass shootings are indeed partially a mental health problem, albeit one poorly addressed by our current laws and policies. But the solution to mass shootings also needs to consider strategies that may reduce gun violence in general.
Nudge or Grudge? Choice Architecture and Parental Decision-Making
First published: 28 March 2018
Abstract
Richard Thaler and Cass Sunstein define a nudge as “any aspect of the choice architecture that alters people’s behavior in a predictable way without forbidding any options or significantly changing their economic incentives.” Much has been written about the ethics of nudging competent adult patients. Less has been written about the ethics of nudging surrogates’ decision-making and how the ethical considerations and arguments in that context might differ. Even less has been written about nudging surrogate decision-making in the context of pediatrics, despite fundamental differences that exist between the pediatric and adult contexts. Yet, as the field of behavioral economics matures and its insights become more established and well-known, nudges will become more crafted, sophisticated, intentional, and targeted. Thus, the time is now for reflection and ethical analysis regarding the appropriateness of nudges in pediatrics.
We argue that there is an even stronger ethical justification for nudging in parental decision-making than with competent adult patients deciding for themselves. We give three main reasons in support of this: (1) child patients do not have autonomy that can be violated (a concern with some nudges), and nudging need not violate parental decision-making authority; (2) nudging can help fulfill pediatric clinicians’ obligations to ensure parental decisions are in the child’s interests, particularly in contexts where there is high certainty that a recommended intervention is low risk and of high benefit; and (3) nudging can relieve parents’ decisional burden regarding what is best for their child, particularly with decisions that have implications for public health.
Patient Care to Public Health to Synthetic Biology
First published: 19 February 2018
Abstract
The January-February 2018 issue of the Hastings Center Report includes pieces addressing patient care concerns that lie at the original core of bioethics and pieces that reflect the field’s growing breadth. Among the pieces getting at the original core is an article by philosopher Daniel Brudney on the moral values underpinning surrogate decision-making. The article and the two commentaries that follow it contribute to the debate on the moral authority of surrogate decision-makers. Several items in the issue take up matters of public health and health policy. For example, the lead article, by Nir Eyal, examines the ethics of using inconvenience—waiting lists and the like—to constrain the consumption of health care services, and a commentary by Lawrence Gostin examines the regulation of sugary beverages. A supplement to the issue contains a special report about the tools and processes used to assess the impact of emerging technologies, with a focus on synthetic biology.
Tackling Obesity and Disease: The Culprit Is Sugar; the Response Is Legal Regulation
First published: 19 February 2018
Abstract
It is staggering to observe the new normal in America: 37.9 percent of adults are obese, and 70.7 percent are either obese or overweight. One out of every five minors is obese. The real tragedy, of course, is the disability, suffering, and early death that devastates families and communities. But all of society pays, with the annual medical cost estimated at $147 billion. The causal pathways are complex, but if we drill down, sugar is a deeply consequential pathway to obesity, and the single greatest dietary source is sugar-sweetened beverages (SSBs). The copious amount of sugar in the American diet is no accident. Industry practices and regulatory failures have fueled this explosion. Yet there are sensible, effective interventions that would create the conditions for healthier behaviors. What are the key interventions, and how can we overcome the social, political, and constitutional roadblocks? Tobacco control offers a powerful model, suggesting that success requires a suite of interventions working in concert: labeling, warnings, taxation, portion sizes, product formulation, marketing restrictions, and bans in high-risk settings such as schools and hospitals. Each intervention deserves detailed analysis, but I’m kick-starting scholarly and policy conversation by systematically laying out the major legal tools.
Raising the Stakes for Nondiscrimination Protections in the ACA
First published: 19 February 2018
Abstract
In the struggle over the durability of the Affordable Care Act, defenders of the ACA stand guard at many fronts. A major contribution of the ACA to nondiscrimination law, however, appears increasingly vulnerable. The ACA established significant new nondiscrimination protections for patients under section 1557 and its implementing regulations. Several of these regulations—including protections on the basis of gender identity and pregnancy termination—are now under reconsideration at the Department of Health and Human Services, after a nationwide injunction lasting almost a year. Nondiscrimination laws matter, of course, because they promote equal access to health care. But focusing on discriminatory behavior alone is a narrow view of the purpose and potential of nondiscrimination rules—and underestimates the stakes of softening section 1557. To evaluate these protections, we must consider not only their impacts on discriminatory behavior but also their behavioral and attitudinal impacts on patients and communities. This is because supportive or stigmatizing rules can exert an expressive effect: laws communicate information about prevailing social norms, they give some norms greater authority by virtue of the state’s support, and they can shape community values. Through these expressive impacts, nondiscrimination laws may affect not only discriminatory behavior in health activities but also the attitudes, beliefs, and decisions of people who are legally protected.
Community Engagement and Field Trials of Genetically Modified Insects and Animals
First published: 19 February 2018
Abstract
New techniques for the genetic modification of organisms are creating new strategies for addressing persistent public health challenges. For example, the company Oxitec has conducted field trials internationally—and has attempted to conduct field trials in the United States—of a genetically modified mosquito that can be used to control dengue, Zika, and some other mosquito-borne diseases. In 2016, a report commissioned by the National Academies of Sciences, Engineering, and Medicine discussed the potential benefits and risks of another strategy, using gene drives. Driving a desired genotype through a population of wild animals or insects could lead to irreversible genetic modification of an entire species. The NASEM report recommends community, stakeholder, and public engagement about potential uses of the technology, and it argues that the engagement should occur as research advances, well before gene drives are deployed. Yet what “engagement” means in practice is unclear. This article seeks clarity on this problem by offering a justification for community engagement and drawing out implications of this argument for the implementation and desired outcomes of community engagement.
Community engagement is essential when it comes to research that would release genetically modified insects or animals into the environment. By contrast, obtaining informed consent from people who live near such a proposed field trial is neither necessary nor sufficient. Drawing on the epistemic and moral arguments for deliberative democracy, I propose two discrete mechanisms of community engagement: community advisory boards and deliberative forums, neither of which has been systematically incorporated into research governance. The proposed mechanisms would engender respect for persons who live near field trials, even when the results of deliberation override some individuals’ preferences. Community engagement foregrounds the community in our thinking about humans’ relationship to nature, and it implies that deciding to release genetically modified insects or animals into the wild ought to be a collective decision, not one made by product developers, policy-makers, private companies, research funders, or scientists alone.
On Nudging Health
First published: 19 February 2018
Abstract
Ideas of nudging, choice architecture, and libertarian paternalism have sparked much controversy. Some find in them a long-sought optimal harmonization of the commitments to beneficent, welfare-increasing influence and to respecting persons, whereas people on the opposite end see in them an especially sinister form of control. One area in which these ideas are of greatest importance is health care, where improving people’s decisions, under the constraint of respect for persons, is a vital concern. Nudging Health: Health Law and Behavioral Economics, edited by Glenn Cohen, Holly Fernandez Lynch, and Christopher Robertson, is the first book dedicated to this important topic. This anthology of twenty-four chapters, with section introductions and a foreword by Cass Sunstein, presents a wide spectrum of perspectives on both the promise and the difficulties in applying choice architecture to health care. The short and readable chapters, written for the book, cover questions of public health law and policy, clinical practice, medical ethics, and political philosophy. They present a synopsis of the types of questions that nudging brings up in health care broadly construed, offer new analyses, and provide much fodder for thought.
Benefit-Cost Analysis and Emerging Technologies
First published: 16 February 2018
Abstract
Emerging technologies are, by definition, full of surprises: developments that we cannot fully anticipate and that might have some bad outcomes as well as good ones. This presents a challenge for anyone trying to make forward-looking policy decisions, including those who apply benefit-cost analysis. BCA is now widely known and used, but it is also widely misunderstood—by many of its advocates as well as its detractors. In this essay, I will begin by examining some of the strengths and weaknesses of BCA as a normative science. Yes, “normative science” is an oxymoron, and the incongruity it speaks to is a source of much of the controversy; BCA is an imperfect answer, but often the best available answer, to the question of how a society should go about making collective but not unanimous choices.
I also want to take a hard look at the question of what we are evaluating. BCA is designed to weigh government actions, to see whether they are in the public interest; it is not designed to evaluate private actions. But if the government action is to approve a private action that otherwise would be prohibited, then the BCA inevitably must evaluate the latter. From the perspective of a government regulator, it is very tempting to shift the burden of proof onto private innovators—to obligate them to seek permission to proceed, and to demonstrate that their proposed actions have acceptable risks and will produce a net social benefit. But such burden-shifting is not merely an administrative convenience; it has serious economic consequences that need to be examined.
Demystifying Evidence-Based Policy Analysis by Revealing Hidden Value-Laden Constraints
First published: 16 February 2018
Abstract
Consider any choice that affects some social policy. A decision that considers evidence will, at its heart, contain some kind of explicit or implicit “because” statement: “We are doing X because the evidence says Y.” But can evidence ever truly speak for itself, in the sense of being reducible to objective utterances that are either correct or in need of correction? Before answering, consider what you’d prefer. Would you rather receive evidence that was free of any value judgments imposed by human actors, that was laden with value judgments that you agree with, or laden with value judgments that you disagree with? The central assertion of this essay is that, throughout policy analysis but especially in assessments of the costs and benefits of regulating versus encouraging new technologies (cost-benefit analysis, or CBA), the first possibility above is a mirage, and the second and third are self-contradictory. Instead, we are overwhelmingly confronted with a fourth possibility: we receive evidence that appears to be (or is deliberately touted as) value neutral but is suffused with hidden value judgments.
In the second part of this essay, entitled “A Guided Tour through Inevitable Value Judgments,” I identify in a systematic way approximately sixty-five value judgments that are routinely (in some cases, invariably) made in CBA, but that are kept hidden. For each judgment, I discuss its genesis as it is most commonly invoked in CBA, explain how it is hidden in plain sight, and offer one or more value judgments that could be made instead of or in addition to the conventional one. The alternative judgments highlight the width of the spectrum of reasonable conclusions an analyst could reach merely by substituting other judgments for the ones currently embedded.
Bringing hidden value judgments to light is doubly valuable. First, it allows discussion to ensue on a level playing field; instead of conclusory statements about what the evidence says, transparency permits statements taking the form of “when channeled through these value judgments, the evidence says this.” Perhaps more importantly, transparency about value judgments permits participants in the discussions to offer interpretations of evidence contingent on there being different value judgments chosen at one or more points in the analysis, interpretations that may suggest that alternative course(s) of action are preferable to the one being championed.
From CBA to Precautionary Appraisal: Practical Responses to Intractable Problems
First published: 16 February 2018
Abstract
The purpose of this essay is to critically review the design of methods for ethically robust forms of technology appraisal in the regulation of research and innovation in synthetic biology. It will focus, in particular, on the extent to which cost-benefit analysis offers a basis for informing decisions about which technological pathways to pursue and which to discourage. A further goal is to consider what (if anything) the precautionary principle might offer in enabling better decisions. And this, in turn, raises questions about why mention of precaution can excite accusations of unscientific bias or irrational, “anti-innovation” extremism. What does the polarized debate tell us about the politics around synthetic biology? In seeking more rigorous, timely, and practical ways to govern these remarkable new technologies, what might we be missing?
The sophistication, diversity, and scope of synthetic biology may seem to make it a rather idiosyncratic area for exploring these general issues. It may seem to be a special case, with the bewildering pace of change amplifying the difficulties. But at root, some of the trickiest issues are just specific instances of familiar and long-standing conundrums in the governance of science and technology. The basic challenge is how to weigh up, for a wide range of potential options, the various pros and cons, as viewed from divergent perspectives, and find a way to justify the best course of action on behalf of society as a whole. This is the central problem addressed by a number of techniques in CBA. On the face of it, synthetic biology seems to present just one more application of these well-established and self-confident prescriptive methods.
But there do emerge several obstinate, even prohibitive, difficulties for CBA. Although they are well acknowledged by the scholarly literature on and around this topic, they are often sidelined in practice. Yet all are central to the case for applying the concept of precaution to a field like synthetic biology. This essay will briefly explore multicriteria mapping, an appraisal method for exploring contrasting perspectives on emerging technologies, as one practical way to address them. The essay focuses on MCM, not because it presents any sort of panacea for appraisal, but because it is illustrative of the concrete implications of precaution. Setting out even just one among potentially many practical alternative methods at least refutes the last-ditch argument that CBA is the only operational choice.
Real-World Evidence, Public Participation, and the FDA
First published: 24 November 2017
Abstract
For observers of pharmaceutical regulation and the Food and Drug Administration, these are uncertain times. Events in late 2016 raised concerns that the FDA’s evidentiary standards were being weakened, compromising the agency’s ability to adequately perform its regulatory and public health responsibilities. Two developments most directly contributed to these fears—the approval of eteplirsen, a treatment for Duchenne muscular dystrophy, against the recommendations of both FDA staff and an advisory committee and the December 2016 signing of the 21st Century Cures Act, which encouraged greater use by the FDA of “real-world” evidence not obtained through randomized controlled trials. The arrival of the Trump administration—with its deregulatory, industry-friendly approach—has only amplified concerns over the future of the FDA. It is too early to know whether the recent developments are truly harbingers of an FDA less likely to prevent unsafe or ineffective products from reaching the market. But elements in the two events—the role of patient narratives in deliberations regarding eteplirsen and the enthusiasm for real-world evidence in the 21st Century Cures Act—raise critical issues for the future of evidence in the FDA’s work. The rigorous, inclusive approach under way to consider issues related to real-world evidence provides a model for a similarly needed inquiry regarding public participation in FDA decision-making.
Public Health Autonomy: A Critical Reappraisal
First published: 24 November 2017
Abstract
The ethical principle of autonomy is among the most fundamental in ethics, and it is particularly salient for those in public health, who must constantly balance the desire to improve health outcomes by changing behavior with respect for individual freedom. Although there are some areas in which there is a genuine tension between public health and autonomy—childhood vaccine mandates, for example—there are many more areas where not only is there no tension, but public health and autonomy come down to the same thing. These areas of overlap are often rendered invisible by a thin understanding of autonomy. Better integrating newer theoretical insights about autonomy into applied ethics can make discussions of public health ethics more rigorous, incisive, and effective. Even more importantly, bringing modern concepts of autonomy into public health ethics can showcase the many areas in which public health and autonomy have the same goals, face the same threats, and can be mutually advanced by the same kinds of solutions.
This article provides a schema for relational autonomy in a public health context and gives concrete examples of how autonomy can be served through public-health interventions. It marshals insights from sociology, psychology, and philosophy to advance a theory of autonomy and coercion that recognizes three potential threats to autonomy: threats to choice sets, threats to knowledge, and threats to preferences.
The Shifting Landscape of Prenatal Testing: Between Reproductive Autonomy and Public Health
First published: 24 November 2017
Abstract
Since the 1970s, prenatal testing has been integrated into many health care systems on the basis of two competing and largely irreconcilable rationales. The reproductive autonomy rationale focuses on nondirective counseling and consent as ways to ensure that women’s decisions about testing and subsequent care are informed and free of undue pressures. It also represents an easily understandable and ethically convincing basis for widespread access to prenatal testing, since the value of autonomy is well established in Western bioethics and widely recognized by funders of health care. In contrast, the public health rationale approaches prenatal testing as designed to reduce the incidence of certain conditions in the population to reduce the burden of disease. This rationale emphasizes the societal consequences of reproduction and the aggregate impact of women’s individual reproductive decisions on the overall health of future populations. In this essay, I argue that, despite what could be seen as a persistent failure to meet the ideals of reproductive autonomy, resisting the public health rationale as a basis for prenatal screening is ethically and pragmatically crucial. I recommend policy mechanisms that can enhance reproductive autonomy at a societal level to support choice at the individual level.
Reproductive Autonomy and Regulation—Coexistence in Action
First published: 24 November 2017
Abstract
On occasion, British in vitro fertilization practitioners look over the ocean to the practice of IVF and embryo research in the United States, wonder why these areas are subject to less regulation than in the United Kingdom, and ask how much less risky and more progressive IVF and embryo research might be if subject to additional federal, or at least state, regulation. To an American audience, imbued with the centuries-old spirit of independence, regulation and autonomy can seem in tension. From a British perspective, there is no necessary conflict. There is no dissent in the United Kingdom from the proposition that individual activities, services, and industries can be regulated and, at the same time, retain and exercise such autonomy as is their right within a safe sphere. From 1994 to 2002, I was the chair of the United Kingdom’s Human Fertilisation and Embryology Authority, which regulates the practice of IVF and embryo research. The existence of the HFEA assures patients that safety and aspects of the practice of assisted reproduction are monitored, leaving them free to choose without worrying about danger, in the same way that the public may take only those drugs that have passed health and safety tests. I would propose that anxious and vulnerable patients do not have more autonomy in a less regulated, market-driven field.
When Public Health Becomes Politicized
First published: 20 September 2017
Abstract
Perhaps nothing symbolizes the current polarized political climate in the United States more than the world of public health. Public health schools and health departments are full of “true believers,” people willing to crusade for any program designed to reduce morbidity and mortality. But in the “real world,” proven programs and strategies—such as gun-control measures, universal vaccination, and improved traffic safety—are routinely thwarted. Why do critics oppose efforts to improve the public’s health? History can provide some answers.
Defending Opioid Treatment Agreements: Disclosure, Not Promises
First published: 24 May 2017
Abstract
In order to receive controlled pain medications for chronic non-oncologic pain, patients often must sign a “narcotic contract” or “opioid treatment agreement” in which they promise not to give pills to others, use illegal drugs, or seek controlled medications from health care providers. In addition, they must agree to use the medication as prescribed and to come to the clinic for drug testing and pill counts. Patients acknowledge that if they violate the opioid treatment agreement (OTA), they may no longer receive controlled medications. OTAs have been widely implemented since they were recommended by multiple national bodies to decrease misuse and diversion of narcotic medications. But critics argue that OTAs are ethically suspect, if not unethical, and should be used with extreme care if at all. We agree that OTAs pose real dangers and must be implemented carefully. But we also believe that the most serious criticisms stem from a mistaken understanding of OTAs’ purpose and ethical basis.
Reconciling Patient Safety and Epistemic Humility: An Ethical Use of Opioid Treatment Plans
First published: 24 May 2017
Abstract
In this issue of the Hastings Center Report, Joshua Rager and Peter Schwartz suggest using opioid treatment agreements as public health monitoring tools to inform patients about “the requirements entailed by undergoing opioid therapy,” rather than as contractual agreements to alter patients’ individual behavior or to benefit them directly. Because Rager and Schwartz’s argument presents suspected OTA violations as a justification to stop providing opioids yet does not highlight the broader epistemic and systemic context within which clinicians prescribe these medications, their proposal may perpetuate a climate of distrust and stigmatization without correcting systemic factors that may have placed patients and others at risk in the first place. Given the context of epistemic uncertainty regarding opioid safety and efficacy, insufficient training for opioid prescribers, and inadequate patient education, I propose replacing OTAs, which have a narrow focus on patient behaviors, with opioid treatment plans, which would promote mutual, collaborative, and shared decision-making on the most appropriate pain management program. An OTP can be ethically justified as a tool to prevent and treat iatrogenic addiction under a specific paradigm—one that adopts a default position of professional epistemic humility and holds all collaborative parties accountable in chronic pain management.
Opioid Treatment Agreements Repurposed—But Who Monitors the Monitors?
First published: 24 May 2017
In this issue of the Hastings Center Report, Joshua Rager and Peter Schwartz reframe the justification for the use of opioid treatment agreements. Instead of documents used to define the roles and responsibilities of doctors and patients to one another in the course of opioid treatment for chronic pain and to describe the risks and benefits of therapy for the individual, OTAs are now proposed for use as “surveillance and monitoring” instruments. As such, they are specifically meant to disclose the risks of opioid therapy and to describe the other processes and tools used to monitor abuse and diversion of medications. Given the crisis of the opioid overdose and death epidemic, along with this repurposing of OTAs as disclosure documents primarily, Rager and Schwartz argue that patient consent is not needed (although desired) and that OTAs should be universally applied in clinical practices. We can all agree on the big picture goal of limiting the number of opioid prescriptions in order to minimize the tragedy of opioid overdose deaths. We disagree, though, about the acceptable level of collateral damage to people in pain who fall victim to fighting the war against the so-called opioid epidemic.
Employer Wellness Programs Challenged in Court
First published: 11 January 2017
Abstract
Many employers faced with rising health care costs have adopted “voluntary” wellness programs that urge employees to engage in various health-promotion activities, such as smoking cessation and weight reduction. In the proper setting, measures to promote a more healthful lifestyle are difficult to question, but there is little compelling evidence that workplace wellness programs have significant, sustained health benefits or substantially reduce health care costs other than through cost-shifting to unhealthy employees. Congressional support for workplace wellness programs has persisted on a bipartisan basis for the last twenty years, and the incentives that current statutes allow employers to offer employees have become strong enough that the voluntariness of the programs has been called into question. In recent months, the battleground has shifted to the courts, where federal regulations and employer practices have been challenged. Three recent or pending cases raise questions about whether the incentives are coercing employees into the programs.
The ACA’s Provision on Nondiscrimination Takes Shape
First published: 21 September 2016
Abstract
The Department of Health and Human Services has issued far-reaching regulations to implement the nondiscrimination requirement of the Affordable Care Act. Now commonly called “Section 1557,” this ACA provision prohibits discrimination by “any health program or activity, any part of which is receiving Federal financial assistance,” on grounds prohibited under previously enacted federal antidiscrimination statutes. The DHHS Office of Civil Rights enforces Section 1557. These new regulations and accompanying commentary give warning of the standards the agency will use in its enforcement efforts. Courts will also give some deference to the DHHS regulations in interpreting the statute in lawsuits by individuals claiming damages against covered health care providers for illegal discrimination under Section 1557. Three central issues are the nature of the rights created in Section 1557 and their relation to the listed federal antidiscrimination statutes, the sorts of health care programs and activities that are covered by Section 1557, and the definition of the personal characteristics, including sexual orientation and gender identity, against which discrimination is prohibited.
Cultivating Synergy in Nursing, Bioethics, and Policy
First published: 21 September 2016
Abstract
Nursing and bioethics have a lot in common because they share concerns about life and death, illness and health, the rights of individuals and communities, ethical patient care, health care delivery, and public health. Nurses and bioethicists contribute to ethical practice, ethics scholarship, and health policy-making in a variety of ways. Some nurses have bioethics education or experience, some bioethicists study or collaborate closely with nurses, and some of us proudly identify as both bioethicists and as nurses. Despite certain shared and interwoven aims, bioethicists and nurses often accomplish their goals in dissimilar ways, have diverse educational and training trajectories as well as distinct roles and responsibilities, and are viewed differently within health care organizations. Yet the work of bioethics and nursing can be, and in my view should more often be, synergistic. That synergism may be especially critical in the arena of health policy and ethics. Nurses can bring extraordinary insights and real-world experiences to the policy table but are not always considered essential contributors.
Creating a Culture of Ethical Practice in Health Care Delivery Systems
First published: 21 September 2016
Abstract
Undisputedly, the United States’ health care system is in the midst of unprecedented complexity and transformation. In 2014 alone there were well over thirty-five million admissions to hospitals in the nation, indicating that there was an extraordinary number of very sick and frail people requiring highly skilled clinicians to manage and coordinate their complex care across multiple care settings. Medical advances give us the ability to send patients home more efficiently than ever before and simultaneously create ethical questions about the balance of benefits and burdens associated with these advances. Every day on every shift, nurses at the bedside feel an intense array of ethical issues. At the same time, administrators, policy-makers, and regulators struggle to balance commitments to patients, families, staff members, and governing boards. Ethical responsibilities and the fiduciary, regulatory, and community service goals of health care institutions are not mutually exclusive; they must go hand in hand. If they do not, our health care system will continue to lose valued professionals to moral distress, risk breaking the public’s trust, and potentially undermine patient care. At this critical juncture in health care, we must look to new models, tools, and skills to confront contemporary ethical issues that impact clinical practice. The antidote to the current reality is to create a new health care paradigm grounded in compassion and sustained by a culture of ethical practice.
Transitional Care: A Priority for Health Care Organizational Ethics
First published: 21 September 2016
Abstract
Numerous studies have revealed that health care transitions for chronically ill older adults are frequently poorly managed, often with devastating human and economic consequences. And poorly managed transitions and their consequences also occur among younger, relatively healthy individuals who have adequate resources and are prepared to advocate on their own behalf. Despite the rich base of research confirming that evidence-based transitional care enhances patients’ experiences, improves health and quality of life, and reduces costs, organizational, regulatory, financial, and cultural barriers have, until recently, prevented widespread adoption of these proven approaches. Provisions of the Affordable Care Act, such as reductions in Medicare payments to hospitals with very high thirty-day rehospitalization rates, have reduced barriers, but uptake of evidence-based transitional care beyond demonstration projects continues to be sporadic and far too slow. With a rich understanding about how to better anticipate and respond to the compelling problems experienced by patients, family caregivers, and health care professionals throughout episodes of acute illness, the time has come to frame transitional care as a system’s ethical responsibility in an aging society. Embedding transitional care within the ethical obligations of a health care system requires the perspectives and involvement of nurses and nursing because of this profession’s integral role in every aspect of care transitions.
Promoting the Health of Families and Communities: A Moral Imperative
First published: 21 September 2016
Abstract
The Hill Burton Act, which was signed into law in 1946 and ended in 1997, was one of the most significant forces that shaped the health care system we have today. Providing grants and loans for the construction and expansion of hospitals across the country, it required beneficiary hospitals to give some amount of uncompensated care to the poor and uninsured in return.
The act not only led to our health care system’s current emphasis on the acute-care hospital as the primary site of health care delivery, but it also had a profound effect on nursing, fully involving the profession in an acute-care world. The act created jobs for nurses at an unprecedented level. There are over 3.4 million nurses in the United States, and in 2013, 63 percent of all nurses worked for hospitals. Nursing education continues to emphasize acute care, despite the calls for shifting the curriculum to more community-based content and experiences that focus on health promotion and wellness for individuals, families, and communities. It is my premise that the nursing profession and all who profess to be committed to promoting health have a moral obligation to help the nation adopt a Hill-Burton Act of the twenty-first century that will focus on building healthy communities, supporting families in ways that promote health, and helping individuals to live healthier lives. This would require a shift in resources from a costly health care system to investing in community development, whether job creation, building safe places to play and exercise, providing access to affordable and nutritious foods, advancing the quality of education, or other approaches to addressing and improving the social determinants of health. Making this kind of investment would speak to the principles of beneficence, least harm, and justice, particularly for socioeconomically stressed communities.
Quarantine Controversy: Kaci Hickox v. Governor Chris Christie
First published: 06 May 2016
Abstract
Nurse Kaci Hickox is among the “Ebola Fighters” honored by Time magazine as its 2014 Person of the Year, having treated Ebola patients in Sierra Leone while volunteering with Médecins Sans Frontieres. When she returned to the United States in October 2014, she was quarantined in New Jersey for three days before returning home to Maine under the terms of a negotiated release. A year later, in October 2015, Hickox filed suit in federal court against Governor Chris Christie and New Jersey health officials, claiming that the quarantine violated her civil rights. Her complaint asserts that New Jersey officials lacked the authority to quarantine her because she did not pose a significant risk of transmission. The lawsuit raises important questions about disease-transmission risk, the inability of science to rule out certain theoretical risks, and the state’s power to quarantine. It also demonstrates that population health depends on respecting individual liberty and using the best available epidemiological data to set public health policy.
A Vaping Matter: E-cigarette Use in Health Care Organizations
First published: 10 November 2015
Abstract
Although there is no federal legislation yet on e-cigarettes, the U.S. Food and Drug Administration proposed regulations in April 2014 that would prohibit sales of e-cigarettes to anyone under eighteen and require that they be approved by the FDA as a tobacco product and carry warning labels for consumers on their packaging. (The proposed regulations have been characterized as conservative, however, because they do not restrict e-cigarettes that are fruit or candy flavored or restrict advertising, which tends to target young consumers.) Only three U.S. states have extended the same restrictions placed on tobacco products to e-cigarettes; however, eighteen states have passed legislation enacting use restrictions on venues such as schools, state property, or workplaces. Until there is applicable legislation at the federal, state, or municipal levels, health care organizations will have to develop institutional policies if they wish to consistently address the use of e-cigarettes by patients and visitors on their property.
A Buyer’s Market? Fixing the Price for Human Ova for Assisted Reproduction
First published: 10 November 2015
Abstract
The Wall Street Journal article “Putting a Price on a Human Egg” triggered extensive media coverage of a rather unusual challenge to payments made to women providing ova for use in assisted reproduction. In Kamakahi v. American Society for Reproductive Medicine and Society for Assisted Reproductive Technologies, plaintiffs claim that ASRM and SART policies adopting limits on such payments violate the federal antitrust prohibition against price fixing.In 2007, an ASRM Ethics Committee Report, confirming a 2000 report, asserted that, “[a]lthough there is no consensus on the precise payment that oocyte donors should receive, at this time sums of $5,000 or more require justification and sums above $10,000 are not appropriate.” SART is an affiliate organization of ASRM and counts as its members 90 percent of the clinics providing assisted reproductive technologies in the United States. SART requires that its members “[adhere] to all ASRM/SART Guidelines including ethical, practice, advertising, and laboratory.” The plaintiffs in Kamakahi claim that the agreement among SART members to abide by the ASRM policy restricts competition among agencies procuring oocytes and produces lower payments than women would otherwise be able to negotiate. It is through the requirement that SART members adhere to ASRM ethical guidelines that ethics goes to market and encounters antitrust law.
Ethicists continue to debate whether payment for oocytes inappropriately commodifies the human body, and ASRM policy consistently refers to their procurement as the “donation process” and to women who participate as “donors.” Nevertheless, in the context of antitrust law, the procurement of oocytes is a business and clearly falls within the reach of antitrust restrictions on business conduct.
Justice Roberts Gets It
First published: 28 September 2015
Abstract
Opponents of the Affordable Care Act have attempted to topple it in court by challenging the legality of two of its three legs. Three years ago, in NFIB v. Sibelius, Chief Justice Roberts narrowly upheld the constitutionality of the individual mandate, in a 5-to-4 decision that characterized the mandate as an optional tax rather than as a regulatory command. This year, on June 25, the health policy community exhaled a giant sigh of relief when the Supreme Court upheld the subsidy leg of the ACA structure. In King v. Burwell, Justice Roberts again wrote the majority opinion (this time for six members that included Justice Kennedy), ruling as a matter of statutory interpretation that subsidies for insurance premiums are available not just through state-based exchanges but also through the federal exchange.
Training in Research Ethics and Standards for Community Health Workers and Promotores Engaged in Latino Health Research
First published: 07 July 2015
Abstract
A model frequently used to implement community-based research involves engaging local community health workers who are trusted members of the community and familiar with local customs, language, and culture. In Spanish-speaking communities, the CHWs are also known as promotores de salud (“health promoters”). Depending on the study design and nature of the research, promotores facilitate research through community outreach, instrument design, participant recruitment, intervention delivery, data collection, and other research-related tasks. In 2000, the National Institutes of Health published a regulation requiring training of “key personnel” named on NIH-supported research involving human subjects. Regardless of whether promotores are technically designated as key personnel on a particular study, they may benefit from training in research ethics. Unfortunately, the educational programs designed for academic researchers in response to the NIH mandate were poorly aligned with the needs of promotores and not suited for learning about human research ethics applied to the community health setting. For example, many promotores in our California-Mexico border region are monolingual Spanish speakers who have no formal academic research training. Therefore, we set out to develop a training alternative appropriate to our local CHWs. In this essay, we provide overviews of the relevant instructional design principles and our formative research process, including examples of key findings.
Ethics of Development Assistance for Health
First published: 05 May 2015
Abstract
In the past three decades, levels of and contributors to global health aid have increased at an unprecedented pace. Development assistance for health—financial contributions from public and private institutions to low- and middle-income countries to help improve health and health systems—nearly quintupled from 1990 to 2012 (from $5.7 billion to $28.1 billion). DAH is now provided by more than one hundred seventy major global health agencies and organizations, 15 percent of which are private entities (such as the Bill and Melinda Gates Foundation), other not-for-profit organizations, and public-private partnerships. Governments are still the largest source for DAH. While increased DAH is essential and welcome, these system developments raise numerous ethical questions. Are the resources sustainable, and do expenditures target correct priorities? Who should decide, and how should these decisions be made?
World Health Organization Reform: Lessons Learned from the Ebola Epidemic
First published: 04 March 2015
Abstract
It was October 2014, and Ebola was raging out of control in Guinea, Liberia, and Sierra Leone. Margaret Chan, the World Health Organization’s director-general, defended the organization against charges that its response was late and ineffective: “We are a technical agency, with governments having first priority to take care of their people.” In January 2015, the WHO executive board undertook a systematic reform of the agency’s performance, and Chan again offered a defense: I followed protocol, leaving it to the Africa office (AFRO) to respond. Yet the three nations could not possibly have stemmed the outbreak alone, and AFRO was known to be dysfunctional.
Ebola represents an inflection point requiring fundamental reform for the WHO. A failure of leadership will impact its status and legitimacy for a generation. Here, I offer five reforms that would transform it and ensure that it fulfills its constitutional mission as “the directing and coordinating authority on international health work.”
Ebola, Quarantine, and the Law
First published: 19 January 2015
Abstract
Judged by the key measures of morbidity and mortality, the United States has been very fortunate in the Ebola outbreak so far. We have had a limited number of cases and only a few fatalities. As of this writing, all of the health care workers who became infected in the United States have recovered, and none of the other nonhealth care contacts of Ebola patients has become infected. Yet by almost any other measure, the response to Ebola in the United States has been a disaster. Among other things, there has been a wealth of misinformation, politicization of public health, public panic, and unnecessary quarantine. There is plenty of blame to go around. But one often overlooked factor that complicated the response to Ebola is American public health law.
Fevered Decisions: Race, Ethics, and Clinical Vulnerability in the Malarial Treatment of Neurosyphilis, 1922–1953
First published: 18 January 2015
Abstract
Syphilis occupies a unique position in the history of U.S. medicine and medical ethics. Given its widespread prevalence and variable presentation, syphilis was a major professional concern among late nineteenth- and early twentieth-century physicians. Syphilis was also at the center of perhaps the most famous example of medical racism in our history, the U.S. Public Health Service Syphilis Study at Tuskegee, in which officials followed the natural history of the disease in a cohort of black men for forty years without offering treatment, even once penicillin became available. In this essay, I call attention to a less well-known aspect of syphilis and its history. I examine one of the disease’s most dreaded manifestations, neurosyphilis (also known as general paresis or general paralysis of the insane), and its treatment via malarial inoculation from the 1920s into the 1950s. The goal of this treatment, dramatic even to observers at the time, was to produce spiking fevers that would kill the syphilitic spirochete and arrest the disease process. My focus will be on developments at St. Elizabeths Hospital, a large-scale federal psychiatric facility in the District of Columbia that served the city’s residents and members of the U.S. military. Physicians at St. Elizabeths were the first in the United States to experiment with malarial fever therapy, treating their initial cohort of patients in December of 1922.
Malarial fever therapy raised a host of ethical questions, rendered all the more complex from today’s vantage point by efforts to understand them within the context of the time. What sorts of risks, both from malaria and via indirect exposure, might be deemed acceptable in the treatment of a devastating and almost invariably fatal disease? How ought researchers and clinicians to have approached the question of consent, itself an evolving concept in the early decades of the twentieth century, when the disease they were targeting impaired a patient’s ability to reason effectively? Finally, at a time when segregated and inferior care for black Americans was the norm and when the black community bore a disproportionate burden of disease, who would have had access to malarial fever therapy, and at what cost?
Public Health Emergencies: What Counts?
First published: 21 March 2014
Abstract
Although Jonathan Herington, Angus Dawson, and Heather Draper offer valuable insights on how to conceptualize health hazards and understand their effects on populations, I resist the label “public health emergency” for obesity, and here is why. It is important—politically and pragmatically—to be judicious with words that have legal and real-world consequences. Once a concept is stretched to encompass a broad swath of events, it loses its power. The broader the application of the term “public health emergency,” the more it loses the core idea of an emergent event. Thus, framing a long-simmering health hazard such as obesity as an emergency would mute the voices of public health authorities seeking a surge response to a truly emergent event, such as a rapidly spreading novel disease or a natural or man-made disaster.
Disingenuous: The Latest Legal Challenges to Insurance Market Reforms
First published: 17 September 2014
Abstract
Not since the civil rights era has enacted national legislation been fought so fiercely as the Patient Protection and Affordable Care Act. Political, ideological, and social forces have mobilized to undermine the ACA at numerous fronts, including the Supreme Court, Congress, state governments, and the court of public opinion. The ACA has survived a constitutional challenge, a presidential re-election, numerous repeal votes in the House, and avowedly obstreperous state regulators. But it has not yet run the full gauntlet of lethal strategies. The latest line of attack is a collection of orchestrated lawsuits seeking to keep the federal exchange from paying any premium tax subsidies.
What if the challengers eventually prevail? What would happen then?
The Ethics of Translating High-Throughput Science into Clinical Practice
First published: 17 September 2014
Abstract
Biomedical research is increasingly data intensive and computational, and “big data science” is migrating into the clinical arena. Unfortunately, ethicists, regulators, and policy-makers have barely begun to explore the ethical, legal, and social issues raised by the variety of analytical and computational approaches in use and under development in biology and medicine. Most scholarship concerning big data bioscience has focused on privacy, a vitally important consideration but not the only one. Among the issues raised by new computational technologies are questions about safety and safety assessment, justice, and how to obtain proper informed consent. These technologies also raise a myriad of regulatory issues that could influence the probability of translating new assays or computational tools to the clinical or public health spheres.
Affordable Access to Care for the Undocumented
First published: 17 September 2014
Abstract
How do you tell a sick kid that nobody cares if he gets better? That’s an exaggeration, of course, but it is the fundamental message our society sends when we tell him that, because he and his family are undocumented immigrants, we are unwilling to extend them access to affordable and reliable health insurance.
One major shortcoming of the Affordable Care Act is its specific exclusion of the almost twelve million undocumented immigrants—including millions of children—in this country from access to the state and federal insurance exchanges where coverage can be purchased. It is true that providing undocumented immigrants access to the exchanges and subsidies mandated by the ACA would require additional funding. However, a recent analysis in California has found that the costs of expanding state-supported care to include undocumented immigrants would largely be offset by the increased state sales tax revenue paid by managed care organizations and by reduced spending at the county level on emergency-room and hospital care of the uninsured.
Reducing Health Disparities and Enhancing the Responsible Conduct of Research Involving LGBT Youth
First published: 17 September 2014
Abstract
Although there is clearly a need for evidenced-based behavioral or biomedical prevention or treatment programs for suicide, substance abuse, and sexual health targeted to members of the LGBT population under the age of eighteen, few such programs exist, due in substantial part to limited research knowledge. Ambiguities in regulations that govern human subjects protections and the related inconsistencies in institutional review board (IRB) interpretations of regulatory language are the key reason for the lack of rigorous clinical trial evidence to support treatment choices and prevention approaches to reducing health disparities for this population. Given the socially sensitive nature of suicide, substance abuse, and HIV and STI research in general and LGBT research specifically, in the absence of empirical data to guide their decisions, IRBs must often rely on subjective judgments of minimal risk, which can lead to overestimation of the magnitude and probability of psychological, social, and informational harms that might arise from LGBT youth participation in clinical trials. In addition, more than other youth, LGBT adolescents whose families are unaware of their sexual orientation or gender identity or whose families have victimized them on account of it may be reluctant to participate in studies that require guardian permission. This, in turn, intensifies problems of recruitment and unbiased sampling. However, many IRBs are reluctant to apply federal regulations permitting waiver of guardian permission under conditions in which such permission is clearly not “feasible” or “reasonable” to require. Consequently, many investigators have excluded LGBT individuals under eighteen years of age in health intervention research proposals because of anticipated or actual difficulties obtaining IRB approval. This situation is in conflict with current ethical discourse focusing on the right of youths to participate in trials that will protect them from receiving developmentally untested, inappropriate, and unsafe treatments. In this article, we describe these barriers and recommendations for providing LGBT youth safe and fair access to health research.
When a Blood Donor Has Sickle Cell Trait: Incidental Findings and Public Health
First published: 09 July 2014
Abstract
There are no national recommendations for routine screening for sickle cell trait, nor is there guidance on whether or how to notify donors that they might be tested or identified as having sickle cell trait. As a result, the organizations that collect blood have implemented variable policies about whether and how to inform prospective donors of the possible screening and discovery of this noncommunicable condition. The question of what they should do is related to the broader question of how to handle incidental and secondary findings. In a recent report, the Presidential Commission for the Study of Bioethical Issues outline a framework for handling such findings in the clinical, research, and direct-to-consumer contexts. While the commission’s report did not directly address incidental and secondary findings in the public health context of blood donation, it made several overarching recommendations that apply in all contexts where such findings might arise. This essay outlines the special issues raised by discovering sickle cell trait in blood donation and considers the implications of the commission’s framework for that problem.
Obesity, Liberty, and Public Health Emergencies
First published: 11 June 2014
Abstract
Widespread obesity poses a serious challenge to health outcomes in the developed world and is a growing problem in the developing world. There has been a raft of proposals to combat the challenge of obesity, including restrictions on the nature of food advertising, the content of prepared meals, and the size of sodas; taxes on saturated fat and on calories; and mandated “healthy-options” on restaurant menus. Many of these interventions seem to have a greater impact on rates of obesity than does simply providing information about health risks and healthier lifestyles. The more interventionist policy options have, however, been implemented only slowly, in large part because of criticisms that they are unjustified infringements on the liberty of consumers. Food industry groups, free-market think tanks, and the popular press regard measures that incentivize or penalize particular food and lifestyle choices as unjustifiable state regulation of purely self-regarding behavior.
To counteract the liberty-oriented position, those who favor a more interventionist role for the state have recently argued for labeling obesity as a public health emergency. By labeling obesity as a public health emergency, policy-makers could override concerns about individual liberty in order to pursue more interventionist policies designed to guide consumer choices toward healthier lifestyles. In this paper, we argue that, contrary to initial appearances, obesity possesses some of the morally relevant features of public health emergencies, though we do not argue that it actually constitutes one.
Tobacco Endgame: The Poverty Conundrum
First published: 12 May 2014
Abstract
There is no more striking public health triumph than the demise of the “brown plague.” The cigarette was once the accoutrement of a good life, but smoking is now a tragic habit of the poor. By the mid-1960s, half of all men and a third of women in the United States smoked. Today the national prevalence is 18 percent, with rates in major cities below 15 percent. A suite of policies drove down smoking rates—antismoking campaigns, taxation, clean air laws, package labeling, and marketing curbs. These policies, and the resultant behavior changes, however, have diminishing returns. Is it possible that tobacco rates will remain relatively stagnant? If so, what “endgame” strategies might drive rates to negligible levels, say, lower than 5 percent? And if society does achieve such an audacious goal, how attentive should it be to the problems of social justice?
Counterterrorism, Ethics, and Global Health
First published: 12 May 2014
Abstract
The intersection of national security, foreign policy, and health has been explored in a number of arenas, but little attention has been devoted to the ethical issues surrounding the global health impact of current counterterrorism policy and practice. In this essay, we’ll review a range of harms to population health traceable to counterterrorism operations, identify concerns involving moral agency and responsibility—specifically of humanitarian health workers, military medical personnel, and national security officials and operatives—and highlight two interrelated policy issues: the need for a conception of national security that incorporates a cosmopolitan concern for health, and the need for shared health governance, including governance of activities affecting health.
Silencing Marcellus: When the Law Fractures Public Health
First published: 14 March 2014
Abstract
We tend to think of conflict as bad and compromise as good. But how should we view conflict that exposes potential threats to the environment and health? And what about a compromise between litigants that may adversely affect the interests of third parties or undermine public health? There can be few places in the country where this issue has become more pressing than in my home state, Pennsylvania. The hydraulic fracturing of natural gas in the Marcellus Shale has transformed lives and landscapes here, mainly in rural communities with low-income populations. The Hallowich family is a case in point.
Fairness, health, and access
First published: 18 November 2013
Abstract
During the past two years, much of my work at The Hastings Center has explored the implementation of health reform in the United States and its implications for poor and vulnerable groups. These projects include a study of access to care for undocumented patients and one that examines state-level decisions about health reform, including Medicaid expansion and the creation of health insurance “marketplaces.” Both raise issues central to bioethics, including fairness, justice, and the stewardship of society’s resources. Our nation spent about 2.7 trillion dollars on health care in 2012, and its major public health insurance programs represent over 20 percent of the federal budget. Despite these investments, there are troubling differences in life expectancy, infant mortality, and premature death depending on factors like income, race, ethnicity, gender, and where people live.
Bloomberg’s Health Legacy: Urban Innovator or Meddling Nanny?
First published: 01 October 2013
Abstract
Michael Bloomberg assumed office as the 108th mayor of New York City on January 1, 2002. As he leaves the mayoralty—having won re—election twice-his public health legacy is bitterly contested. The public health community views him as an urban innovator—a rare political and business leader willing to fight for a built environment conducive to healthier, safer lifestyles. To his detractors, Bloomberg epitomizes a meddling nanny—an elitist dictating to largely poor and working—class people about how they ought to lead their lives. His policies have sparked intense public, corporate, and political ire—critical of sweeping mayoral power to socially engineer the city and its inhabitants.
Here, I seek to show how Bloomberg has fundamentally changed public health policy and discourse. He has used the engine of government to make New York City a laboratory for innovation-raising the visibility of public health, testing policy effectiveness, and probing the boundaries of state power. Even though the courts have blocked some of his boldest initiatives, he has offered a paradigm for the “new public health”—reaching beyond infectious diseases to upstream risk factors in everyday life and the human habitat. I also critically probe various arguments designed to derail his policies, along with the overarching charge of unjustified paternalism.
Preventing Sin: The Ethics of Vaccines Against Smoking
First published: 06 May 2013
Abstract
The alarming rates of smoking, obesity, and substance abuse pose an enormous challenge for parents and public health officials: how do we prevent children and adolescents from adopting unhealthy behaviors? One new option that may soon be available is the use of nicotine vaccines. Immunological therapies to help smokers stop smoking have shown promise in phase I and II trials; similar therapies could combat smoking addiction before it starts. Nicotine vaccines are distinctive because they confer protection not against infection—the normal target for vaccines—but against enticing pleasures that lead to unhealthy behaviors. As a result, using them preventively in children would be likely to arouse some novel ethical concerns that should be addressed before the vaccines become commonly available and their off-label use as a preventive measure becomes a real option.
In this paper, we consider whether it would be ethical for parents to vaccinate their children against smoking if a nicotine vaccine were to be proven effective as a preventive intervention for children or adolescents. We begin by explaining the current state of nicotine vaccine science and suggesting some likely ethical concerns about allowing parents to have their children receive a vaccine. We then present a preliminary argument for making vaccination permissible, at least if nicotine vaccination substantially reduces the probability that someone subsequently becomes a smoker. We consider a series of possible ethical objections, which are useful for identifying the conditions under which it would be ethical for parents to vaccinate their children against smoking. We conclude that it would be permissible for parents to give their child a nicotine vaccine if the following conditions were met: the vaccine is expected to result in a net benefit to each individual vaccinated, the expected harms from the side effects of the vaccine are lower than the nonvoluntary harms caused by smoking, and there are no other, less manipulative methods available that are as effective at preventing smoking initiation.
Exchanges on Obesity and Smoking
First published: 06 May 2013
Abstract
The January-February issue of the Report introduced a number of new features designed to provide opportunities for further give-and-take in our pages. In this issue, we put to use our revamped letters to the editor, Exchange, with a set of commentaries on another of the January-February articles, Daniel Callahan’s “Obesity: Chasing an Elusive Epidemic.” Commentaries in Other Voices and special reports are planned and solicited, in consultation with scholars in the field and with the guest editors of the special reports, but our hope is that Exchange will provide an opportunity for unsolicited voices in the Report. Of course, Callahan’s controversial article is all too good for drumming up unsolicited commentary: Callahan argued that the rise in obesity requires an aggressive public health campaign that employs some stigmatization of obesity.
“Enhanced, Edgier”: A Euphemism for “Shame and Embarrassment”?
First published: 06 May 2013
Abstract
One of six commentaries on “Obesity: Chasing an Elusive Epidemic,” by Daniel Callahan, from the January-February 2013 issue.
If Shaming Reduced Obesity, There Would Be No Fat People
First published: 06 May 2013
Abstract
One of six commentaries on “Obesity: Chasing an Elusive Epidemic,” by Daniel Callahan, from the January-February 2013 issue.
Obesity Stigma: A Failed and Ethically Dubious Strategy
First published: 06 May 2013
Abstract
One of six commentaries on “Obesity: Chasing an Elusive Epidemic,” by Daniel Callahan, from the January-February 2013 issue.
Good and Bad Ideas in Obesity Prevention
First published: 06 May 2013
Abstract
One of six commentaries on “Obesity: Chasing an Elusive Epidemic,” by Daniel Callahan, from the January-February 2013 issue.
National Obesity Rates: A Legitimate Health Policy Endpoint?
First published: 06 May 2013
Abstract
One of six commentaries on “Obesity: Chasing an Elusive Epidemic,” by Daniel Callahan, from the January-February 2013 issue.
Obesity and Blame: Elusive Goals for Personal Responsibility
First published: 06 May 2013
Abstract
One of six commentaries on “Obesity: Chasing an Elusive Epidemic,” by Daniel Callahan, from the January-February 2013 issue.
A “Fair Use” Exception for Public Health Uses of Medical Information?
First published: 06 May 2013
Abstract
Should public health authorities have access to your personal medical information without your permission? The usual justifications for requiring informed consent do not necessarily apply. That is not to say that consent may be avoided in all situations, just that the reasons for requiring consent in public health are different than for traditional medical treatment.
Drug Compounding, Drug Safety, and the First Amendment
First published: 12 March 2013
Abstract
In September 2012, news broke of a developing drug disaster in the United States. Health authorities had linked a fungal meningitis outbreak to a contaminated steroid made by a company called the New England Compounding Center. The contaminated steroid was a compounded drug that had not been approved by the Food and Drug Administration, differing from three others that had been approved in that it lacked preservatives present in those agents. Factory inspections revealed unsanitary conditions at NECC’s drug production facility. By the time the source of the outbreak was identified, an estimated fourteen thousand people had been injected with the drug. As of December 2012, thirty-nine had died of meningitis, and hundreds more had been diagnosed with meningitis and other drug-related conditions.
Many factors contributed to this disaster. One was a 2002 Supreme Court decision holding that a law prohibiting providers of compounded drugs from promoting their products through advertising and other means impermissibly restricted commercial speech.
The Undocumented Unwell
First published: 11 January 2013
Abstract
Nell Toussaint is not well. In recent years, she has been diagnosed with uterine fibroids, uncontrolled hypertension, nephrotic syndrome, poorly controlled diabetes, hyperlipidemia, and a pulmonary embolism. She also suffers from decreased mobility, shortness of breath, and-perhaps not surprisingly, given her other ailments-anxiety. Toussaint is an indigent undocumented immigrant living in Canada who has been trying to secure medical coverage in the federal courts. In the process, she has sacrificed the medical confidentiality that most of us ordinarily enjoy.
Toussaint first came to Canada from Grenada as a visitor in 1999 and remained after the term of her visa expired. At first, she earned enough to sustain a living, but in 2006, her health began to deteriorate, and she was no longer able to work. Although she has received some medical care since then, it has been sporadic, on an emergency basis, and at great expense. When Toussaint applied for medical health coverage under Canada’s Interim Medical Health Program, which covers the cost of emergency medical care for legally admitted indigents, her application was rejected. She challenged the decision in federal court on the grounds that her right to life and security of the person under the Canadian Charter had been violated and that the denial of coverage was discriminatory.
Obesity: Chasing an Elusive Epidemic
First published: 18 December 2012
Abstract
Obesity may be the most difficult and elusive public health problem this country has ever encountered. Unlike the classical infectious diseases and plagues that killed millions in the past, it is not caused by deadly viruses or bacteria of a kind amenable to vaccines for prevention, nor are there many promising medical treatments so far. While diabetes, heart disease, and kidney failure can be caused by obesity, it is easier to treat those conditions than one of their causes. I call obesity elusive partly because of the disturbingly low success rate in treating it, but also because it requires changing the patterns, woven deeply into our social fabric, of food and beverage commerce, personal eating habits, and sedentary lifestyles. It also raises the most basic ethical and policy questions: how far can government and business go in trying to change behavior that harms health, what are the limits of market freedom for industry, and how do we look upon our bodies and judge those of others?
Lessons to Improve the Efficiency and Equity of Health Reform
First published: 13 September 2012
Abstract
The recent Supreme Court decision on several provisions of the Patient Protection and Affordable Care Act provides an opportunity to address two kinds of design flaws in the legislation whose correction would both improve economic efficiency and some important dimensions of equity.
The Court’s view that the mandate is a tax is consistent with the general economic view that defines a tax as “a compulsory payment for public purposes.” This was the viewpoint I took in my earlier work as well. However, there is considerable difference, disagreement, and ambiguity about the public purpose sought by the ACA payment. The primary purpose of the mandate in my work and in arguments for the mandate in Massachusetts was to try to get as many people as possible to have at least some insurance coverage. A secondary consequence of a mandate is to shore up community rating, although community rating per se does not contribute (and generally is harmful) to the goal of covering a greater proportion of the population.
Child Safety, Absolute Risk, and the Prevention Paradox
First published: 25 April 2012
Abstract
Imagine you fly home from vacation with your one-and-a-half-year-old son who is traveling for free as a “lap child.” In the airport parking lot, you put him into his forward-facing car seat, where he sits much more contentedly than he did in the rear-facing one that was mandatory until his first birthday. After he falls asleep on the way home, you transfer him to his crib without waking him, lowering the side rail so you can lift him in more easily.
Many parts of this idyllic parenting picture are deemed unacceptably risky according to recent child safety proposals. While these proposals all aim to improve child safety, their possible impact is unclear because there has been little discussion of the absolute risk and risk reduction involved in each. And while precise figures are lacking, rough estimates indicate that the magnitudes are quite small. I will argue that this risk and benefit data raises important questions about the proposals, including whether parents might reasonably believe that the small absolute risk reduction offered by the proposed changes does not justify the attendant burdens. This possibility—termed the “prevention paradox” in other contexts—highlights ethical and theoretical challenges in this area of public health.
Ethical and Political Challenges to Seeking Social Justice
First published: July 2008
Abstract
Childhood obesity may have severe long-term consequences for health—indeed, for the overall course of a person’s life. Do these harms amount to a problem of social justice? And if so, what should be done about it? Parents are usually granted considerable leeway to make decisions that affect their children’s health. Social and moral theory has often overlooked the family, however, leaving us with an inadequate understanding of parental autonomy and of how social policy may influence it.
Health Care and Equality of Opportunity
First published: March 2007
Abstract
One widely accepted way of justifying universal access to health care is to argue that access to health care is necessary to ensure health, which is necessary to provide equality of opportunity. But the evidence on the social determinants of health undermines this argument.
Justice and the Human Development Approach to International Research
First published: January 2005
Abstract
The debate over when medical research may be performed in developing countries has steered clear of the broad issues of social justice in favor of what seem more tractable, practical issues. A better approach will reframe the question of justice in international research in a way that makes explicit the links between medical research, the social determinants of health, and global justice.
The Smallpox Vaccination of Health Care Workers: Professional Obligations and Defense against Bioterrorism
First published: September 2003
Abstract
Health care workers have not gone along with President Bush’s request that they be vaccinated against smallpox in order to prepare the nation’s health care system for a terrorist attack using the virus. But there is no professional moral obligation to receive the vaccination—either as a matter of public health or as a matter of national security.
Policy as Product: Morality and Metaphor in Health Policy Discourse
First published: May 1999
Abstract
Where we once spoke in military terms, we now often wield the language of the market: health care is a “product” and we are its “providers” and “consumers.” The market metaphor constrains in various ways our vision of the goals we pursue in making health policy, of the options available to us in pursuing them, indeed—because policy implies a certain view of moral agency—of the way we relate to each other.
From The Hastings Center Bioethics Timeline:
1946: Hill-Burton Act
Congress enacted the Hospital Survey and Construction Act (Hill-Burton Act), which provides for hospitals, nursing homes, and other health facilities grants and loans for construction and modernization. Intended to insure 4.5 hospital beds per 1,000 people, the Act made hospital care more readily available in many parts of the United States.
1946: Guatemala Syphilis Studies
The Syphilis Study Section of the National Institutes of Health-approved grants for Public Health Service researchers to study intentional infection with syphilis, gonorrhea, and chancroid, followed by treatment with newly available penicillin. The studies, involving more than 1,300 Guatemalan soldiers, prisoners, and mental patients, began in 1946 and ended in 1948. The studies remained buried in the archives until 2010.
1962: Congress Passes Kefauver-Harris Amendment
The Kefauver-Harris amendment to the Federal Food, Drug and Cosmetic Act, which mandated safety and efficacy testing prior to the marketing of drugs, is passed by Congress. It was written in response to the Washington Post’s front-page expose of the thalidomide tragedy, in which about 8,000 infants with missing or malformed limbs were linked to thalidomide’s widespread usage among pregnant women (mostly in Europe) after having taken the drug for nausea.
1964: Surgeon General’s Report on Smoking
Surgeon General Luther Terry issues Smoking and Health, a report using epidemiological studies to demonstrate that cigarette smoking caused lung cancer and likely heart disease. This was a landmark study in both the history of public health and health activism.
1965: Letter Questioning Tuskegee Study
Detroit physician Irwin Schatz writes to the U.S. Public Health Service questioning the morals of the Tuskegee Study of Untreated Syphilis in the Negro Male, but his letter is ignored. Seven years later, there would be widespread outrage when details of the study went public.
1965: Congress Passes Medicaid and Medicare
Despite opposition from the American Medical Association, two governmental health insurance programs are passed: Medicaid, which insures the indigent, and Medicare, which insures those 65 and older. The implementation of Medicare, along with the 1963 Fourth Circuit Court of Appeals case mandating desegregation of hospitals and linking desegregation with federal funding policies, transformed hospitals from among the most segregated to the most integrated institutions in the nation. The National Medical Association, which represents the interests of African American patients and physicians, supported both Medicaid and Medicare.
1971: Publication of John Rawls’ A Theory of Justice
John Rawls proposes a theory of justice that provides an alternative to utilitarian theories of justice and addresses concerns about the distribution of benefit. His theory is a form of social contract theory. While his work does not address health policy, it profoundly influences subsequent ethical analysis regarding the fair distribution of health care and other health-related interventions.
J. Rawls, A Theory of Justice (Harvard University Press, 1971)
1972: Tuskegee Syphilis Study Revealed
The study of “Untreated Syphilis in the Negro Male” was begun by the U.S. Public Health Service in 1932. In the mid-1960s, Peter Buxton, a PHS venereal disease investigator in San Francisco, found out about the Tuskegee study and expressed concerns to his superiors that it was unethical. The PHS formed a review committee but ultimately opted to continue the study with the goal of tracking participants until all had died so that autopsies could be performed and project data could be analyzed. Buxton then leaked the story to a reporter friend who passed it on to a fellow reporter. Jean Heller of the Associated Press broke the story in July 1972, prompting public outrage and forcing the study to shut down.
J. Heller, “Syphilis Victims in U.S. Study Went Untreated for 40 Years,” New York Times, July 26, 1972. https://www.nytimes.com/1972/07/26/archives/syphilis-victims-in-us-study-went-untreated-for-40-years-syphilis.html
1973: Patient’s Bill of Rights
1973: Final Report of the Tuskegee Syphilis Study Ad Hoc Advisory Panel Is Submitted to the U.S. Public Health Service
The Advisory Panel described the study as ethically unjustified and recommended that a permanent national board be established with authority to regulate federally supported research involving human subjects.
https://biotech.law.lsu.edu/cphl/history/reports/tuskegee/complete%20report.pdf
1976: Ebola Outbreak
In 1976, the first cases of Ebola virus were discovered near the Ebola River in Zaire (now known as the Democratic Republic of Congo). From the moment of its discovery until the present day, the disease has been a focus of controversy as narratives about scientific triumphalism conflicted with anthropological observations of cultural imperialism in the guise of science. Although indigenous cultural beliefs and practices were blamed for preventing effective treatment of the disease, a major cause of the virus’s spread turned out to be improper sterilization of needles, i.e., so-called scientific medicine. The outbreak was ultimately contained by traditional epidemiological methods of contact tracing, isolation, and quarantine.
https://www.sciencemag.org/news/2014/08/part-one-virologists-tale-africas-first-encounter-ebola
https://www.sciencemag.org/news/2014/08/part-two-virologists-tale-africas-first-encounter-ebola
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(14)62382-5/fulltext
1981: Gay-Related Immunodeficiency (GRID), later redubbed AIDS
Acquired Immune Deficiency Syndrome is recognized by the U.S. Centers for Disease Control (CDC).
https://www.nytimes.com/1982/05/11/science/new-homosexual-disorder-worries-health-officials.html
1985: Public Health Service Task Force Report on Women’s Health Issues
The first federal effort to examine women’s health issues which recognizes that women have different health issues than men. It led to the inclusion of women in human subject’s research.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1424718/pdf/pubhealthrep00101-0075.pdf
1985: Heckler Report
Report of the Secretary’s Task Force on Black and Minority Health resulted in the creation of the Office of Minority Health in the Office of Health and Human Services.
https://www.ahrq.gov/research/findings/nhqrdr/chartbooks/blackhealth/part2.html
1995: Ebola Outbreak
In 1976, the first cases of Ebola virus were discovered near the Ebola River in Zaire (now known as the Democratic Republic of Congo). From the moment of its discovery until the present day, the disease has been a focus of controversy as narratives about scientific triumphalism conflicted with anthropological observations of cultural imperialism in the guise of science. Although indigenous cultural beliefs and practices were blamed for preventing effective treatment of the disease, a major cause of the virus’s spread turned out to be improper sterilization of needles, i.e., so-called scientific medicine. The outbreak was ultimately contained by traditional epidemiological methods of contact tracing, isolation, and quarantine.
https://www.sciencemag.org/news/2014/08/part-one-virologists-tale-africas-first-encounter-ebola
https://www.sciencemag.org/news/2014/08/part-two-virologists-tale-africas-first-encounter-ebola
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(14)62382-5/fulltext
2006: Publication of Madison Powers and Ruth Faden’s Social Justice: The Moral Foundations of Public Health and Health Policy
In their book, Powers and Faden bring our attention to the principle of justice in securing public health and designing health policy. They point out the nondistributional aspects of justice.
M. Powers and R. Faden, Social Justice: The Moral Foundations of Public Health and Health Policy(New York: Oxford University Press, 2006). https://global.oup.com/academic/product/social-justice-9780195375138?cc=us&lang=en&
2006: Approval of the Human Papilloma Virus Vaccine
This vaccine is first approved and may prevent up to 90% of cervical cancers. This first vaccine to protect women against cervical cancer received an expedited review through a priority review process.
https://www.cancer.gov/about-cancer/causes-prevention/risk/infectious-agents/hpv-vaccine-fact-sheet
2006: Publication of Sudhir Anand, Fabienne Peter, and Amartya Sen’s Public Health, Ethics, and Equity
This edited volume recognizes the importance of equity in public health ethics. It provides an interdisciplinary understanding of health equity and promotes the recognition of ethical issues in public health. It includes contributions from philosophers, anthropologists, economists, and public-health specialists on five major themes: defining health equity, health equity and social justice, responsibilities for health, and ethical issues in health evaluation.
S. Anand, F. Peter, and A. Sen, Public Health, Ethics, and Equity (Oxford: Oxford University Press, 2006). https://global.oup.com/academic/product/public-health-ethics-and-equity-9780199276370?cc=us&lang=en&
2010: The Patient Protection and Affordable Care Act
The Patient Protection and Affordable Care Act was signed into law by President Obama on March 23, 2010. One of its principal aims was to expand insurance coverage to millions of uninsured Americans.
Patient Protection and Affordable Care Act, 42 U.S.C. § 18001 et seq. (2010).
www.healthcare.gov/where-can-i-read-the-affordable-care-act/
www.ehealthinsurance.com/resources/affordable-care-act/history-timeline-affordable-care-act-aca
2010: Founding of the Patient-Centered Outcomes Research Institute (PCORI)
The U.S. Congress authorizes the creation of PCORI, an independent nonprofit nongovernmental organization to improve the quality and relevance of evidence to help patients, caregivers, and clinicians to make better-informed health care decisions. The creation of PCORI reflects a shift towards empowering patients by giving them a more active role in making decisions about their care and managing their own health.
2019: Novel Coronavirus (SARS-CoV-2) Outbreak in Wuhan, China
The outbreak of the 2019 coronavirus disease (COVID-19) was first reported on December 31, 2019 in Wuhan China.
2020: Coronavirus (SARS-CoV-2) Pandemic
Massive outbreaks of Covid-19 (the illness caused by SARS-CoV-2) arise initially in China, rapidly becoming a pandemic, overwhelming health systems in Italy, Iran, Spain, and Brazil, as well as New York, California, Florida, Texas, Arizona, and many other countries, states, and cities. Resource shortages prompt development and implementation of plans for contingency and crisis standards of care. The latter were rarely implemented, despite apparent need, which forced consideration of public health ethics and ethically justifiable strategies to allocate scarce resources, such as ICU beds and mechanical ventilators, often focusing on the role of equity. Debates also arise around the relative value and costs of nonpharmaceutical interventions, especially “social distancing” measures such as masking, quarantine, and economic shutdowns. Extreme examples of racial, ethnic, and socioeconomic disparities in Covid-19 infection rates and outcomes are also reported. Though these disparities were not surprising given longstanding, well-documented underlying disparities in health care, they draw particular attention as they are reported at almost the same time as the emergence of widespread protests over racial injustice in policing, sparked by the murder of George Floyd (see below).
2020: Black Lives Matter Movement (George Floyd protests)
Created in 2013 in response to the death of Trayvon Martin and subsequent acquittal of his killer, the Black Lives Matter movement in 2020 becomes a massive “international response to state-sanctioned violence and anti-Black racism,” galvanizing around the videotaped, brutal killing of an unarmed black man named George Floyd by police officers in Minneapolis. Protests over police killings sweep many U.S. cities and the focus quickly expands to encompass racial injustice (and anti-Black racism in particular) in health care and other areas where the legacy of “scientific racism” perpetuates white privilege and structural discrimination again Black and brown people.