Disaster Planning and Bioethics
Selected resources from The Hastings Center.
Bioethics Briefings:
Disaster Planning and Public Health Bioethics Briefing
A public health emergency exists when the health consequences of a decision have the potential to overwhelm routine community capabilities to address them. Public health emergencies may require priority setting, rationing, and triage—which may involve coercive measures that override individual liberty and property rights. Key questions to ask about emergency preparedness planning and emergency response measures are their goals, their effectiveness, and their fairness. Read our briefing to consider: What makes an emergency plan ethically acceptable?
From Hastings Bioethics Forum:
- Pathogens and HumansIn a 1988 essay on pandemics, Nobel laureate Joshua Lederberg wrote, “We have no guarantee that the natural evolutionary competition of viruses with the human species will always find ourselves the winner.”
- WHO-China Report on Covid: Important Step Forward, More to Be DoneThe World Health Organization recently released a long-anticipated report on SARS-CoV-2 origins, based on 28 days of field research and site visits in China…
- Resisting Public Health Measures, Then and NowOne of the most surprising aspects of the Covid-19 pandemic for those of us who teach the history of public health is how unwilling many Americans have been to adopt health measures to protect others. Over the Thanksgiving holiday, tens of millions of Americans traveled, despite the fact that the Centers for Disease Control and Prevention urged them to stay home and the overall death rate from the coronavirus is approaching 300,000. Should recent events make us revisit aspects of the history of public health? And how can these stories inform future public health efforts during pandemics?
- Social-Change Games Can Help Us Understand the Public Health Choices We FaceBefore there was the Covid-19 pandemic, there was Pandemic. This tabletop game, in which players collaborate to fight disease outbreaks, debuted in 2007. Expansions feature weaponized pathogens, historic pandemics, zoonotic diseases, and vaccine development races. Game mechanics modelled on pandemic vectors provide multiple narratives: battle, quest, detection, discovery. There is satisfaction in playing “against” disease–and winning. Real pandemic is not as tidy as a game. But can games support understanding about the societal challenges we now face? Yes.
- Cracks in the System: Lessons Learned from the Covid-19 PandemicThe United States leads the world in coronavirus cases and deaths. Although many people have called out the inadequacies of our health care system, Covid-19 has exposed the most significant shortcomings. The need for change can no longer be ignored. Here are three lessons from this pandemic that should be leveraged for change.
- Measure Twice and Cut Once: The Value of Health Care Ethicists in the PandemicThe major success story of health care ethicists in the pandemic has been their role in establishing ventilator triage policies. But they have more to offer the C-suite of health care institutions.
- Beyond the Covid Crisis—A New Social Contract with Public HealthCovid-19 is teaching us the stern lesson that economic well-being and health justice are two sides of the same coin. To weather pandemics and restore the social contact that economic life demands, we need to sign a new social contract with public health.
- Please Don’t (Need to) Use My WorkI helped develop guidelines for the ethical allocation of scarce resources during a public health emergency, such as a pandemic..I hope my contributions have an impact. I especially hope to see my work used since it emphasizes the perspectives of minority and underserved communities, who tend to have less voice in health policy. But now I find myself dreading the use of my work.
- Crowdfunding for Covid-Related Needs: Unfair and InadequateOne-third of all new GoFundMe campaigns in the United States are for COVID-19-related needs. This shows where we have failed as a society. It is a makeshift response to institutional failures and not a fair or sustainable solution to crises.
- COVID-19 and the Global Ethics FreefallSince the initial outbreak in Wuhan last December, the national and global responses to COVID-19 have been in ethics freefall.
- COVID: Collective of Voices in Distress
- Coronavirus and the Crisis of TrustInfluenza and coronavirus cause similar symptoms probably through similar modes of transmission. What is unique about coronavirus is that misinformation, missteps, conspiracies, and cover-ups have left their mark on public trust.
- After Hurricane Harvey, Injustice in HoustonHurricane Harvey dissipated in September, but much of the destruction that it wreaked on Texas and Louisiana remains. When addressing residential concerns, disaster relief…
- Responding to Zika: Ethical Challenges of Zoonotic DiseasesThe World Health Organization will hold an emergency committee meeting on the pandemic reemergence of Zika virus and the explosive increase in reported cases of…
- Responding to Ebola: Fostering Transparency and InclusivityMedia reports indicate that seven individuals have received ZMapp to date, two of whom have died. The first recipients were two American health care…
- Lessons from Ebola: Presidential Bioethics Commission Releases Recommendations on Preparedness for Public Health EmergenciesThis week the Presidential Commission for the Study of Bioethical Issues released a brief, Ethics and Ebola: Public Health Planning and Response,to the administration and…
- Measles, Vaccination, and the Tragedy of the CommonsAfter having been virtually eliminated in the United States in the year 2000, measles have made a comeback, with nearly 150 cases in 17 states…
- Vaccine Exemptions and the Church-State ProblemThe current measles outbreak has brought public attention to the ease with which vaccine exemptions are available. As the media continually inform us, 48…
- Responding to Ebola: Health Care Professionals’ Obligations to Provide CareAs health care institutions in the United States prepare for Ebola patients, many have adopted the policy that those providing hands-on care should come…
- Responding to Ebola: Misplaced Police PowersA number of states have recently adopted mandatory quarantine measures, including New York and New Jersey, for any individual entering the United States who had direct contact…
- Responding to Ebola: The Question of QuarantineDr. Craig Spencer, the first person in New York confirmed to have Ebola, is a clearly dedicated and selfless physician who worked for Doctors…
- Responding to Ebola: Questions about ResuscitationWhile details of the deaths of patients in Dallas and Madrid from Ebola are not public, their passing prompts questions about resuscitation in individuals…
- Responding to Ebola: Retrofitting Governance SystemsIn a recent New York Times op-ed, David Brooks observes that governance, in the form of multilateral organizing, is missing from the response to the Ebola…
- Responding to Ebola: Organizational Ethics, Frontline PerspectivesBeyond crucial questions of fair access to scarce supplies of the experimental drug ZMapp and to other potentially effective drugs to treat Ebola, commentators…
- Responding to Ebola: Selected Commentaries on Key Ethical QuestionsThe Ebola outbreak in West Africa is the largest and deadliest on record, and the crisis is evolving rapidly. More than 2,200 people have been…
- New York’s Measles Outbreak: Take Off Your Shoes and Roll Up Your SleeveToday’s New York Times reported a rare outbreak of measles in New York City. Because the disease was mostly eradicated by 2000, most clinicians were baffled by…
- Romanian Orphans: A Reconsideration of the Ethics of the Bucharest Early Intervention ProjectRecently I had a Susan Reverby moment. Reverby is the Wellesley historian best known for unearthing the revelations of the Guatemalan syphilis and gonorrhea studies conducted…
From Hastings Center Report:
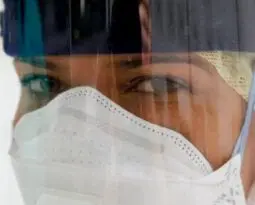
Distressed Work: Chronic Imperatives and Distress in Covid-19 Critical Care
First published: 24 February 2023
Abstract
This ethnographic study introduces the term “distressed work” to describe the emergence of chronic frictions between moral imperatives for health care workers to keep working and the dramatic increase in distress during the Covid-19 pandemic. Interviews and observant participation conducted in a hospital intensive care unit during the Covid-19 pandemic reveal how health care workers connected job duties with extraordinary emotional, physical, and moral burdens. We explore tensions between perceived obligations of health care professionals and the structural contexts of work. Key findings cluster around the moral imperatives of health care work and the distress that work engendered as work spaces, senses of vocation, patient and family interactions, and end-of-life care shifted. While the danger of working beyond limits has long been an ordinary feature of health care work, it has now become a chronic crisis. Assessing this problem in terms of distressed work and its structural contexts can better address effective, worker-informed responses to current health care labor dilemmas.
Zoonoses and Animal Culling: The Need for One Health Policy
First published: 13 October 2022
Abstract
One Health (OH) as a biomedical and social movement calls to reorient public health approaches toward more holistic, nonanthropocentric approaches that do not exclude the interests of animals and ecosystems. OH thus urges reexamination, from both scientific and moral perspectives, of the practice of culling pet, farm, or wild animals in the face of a zoonosis. Pandemics such as Covid and monkeypox highlight the need for more rigorous analysis of the justifications traditionally provided to back these culling practices. Such analyses should then ground reasonable OH policies and legislation that consider the rights of humans, animals, and the environment. Bill S.861, “Advancing Emergency Preparedness through One Health Act of 2021,” which was introduced in the U.S. Congress, is a step in the right direction.
Risk Trade-Offs and Equitable Decision-Making in the Covid-19 Pandemic
First published: 10 February 2022
Abstract
Since the start of the Covid-19 pandemic, societies have faced agonizing decisions about whether to close schools, shutter businesses, delay nonemergency health care, restrict travel, and authorize the use of emergency Covid-19 countermeasures under limited scientific understanding. When both action and inaction can result in significant harm and irreversible damage, decisions surrounding infection control measures become complicated. Yet ethics can help us think about hard trade-offs that weigh competing values and have deep consequences for society and particularly the most disadvantaged. This essay discusses the challenges of making policy trade-offs amid scientific uncertainty. While there may be no perfect formula for deciding what to do and when, we propose four key considerations for assessing risk-risk trade-offs and apply those considerations to the areas of education, economies, health care, travel and migration, social engagement, and medical countermeasures.
Allocation of Opportunities to Participate in Clinical Trials during the Covid-19 Pandemic and Other Public Health Emergencies
First published: 15 December 2021
Abstract
Covid-19 raised many novel ethical issues including regarding the allocation of opportunities to participate in clinical trials during a public health emergency. In this article, we explore how hospitals that have a scarcity of trial opportunities, either overall or in a specific trial, can equitably allocate those opportunities in the context of an urgent medical need with limited therapeutic interventions. We assess the three main approaches to allocating trial opportunities discussed in the literature: patient choice, physician referral, and randomization/lottery. As, we argue, none of the three typical approaches are ethically ideal for allocating trial opportunities in the pandemic context, many hospitals have instead implemented hybrid solutions. We offer practical guidance to support those continuing to face these challenges, and we analyze options for the future.
Life-Years & Rationing in the Covid-19 Pandemic: A Critical Analysis
First published: 16 September 2021
Abstract
Prominent bioethicists have promoted the preservation of life-years as a rationing strategy in response to the Covid-19 pandemic. Yet the philosophical justification for maximizing life-years is underdeveloped and has a complex history that is not reflected in recent literature. In this article, we offer a critical investigation of the use of life-years, arguing that evidence of public support for the life-years approach is thin and that organ transplantation protocols (heavily cited in pandemic-response protocols) do not provide a precedent for seeking to save the most life-years. We point out that many state emergency-response plans ultimately rejected or severely attenuated the meaning of saving the most life-years, and we argue that philosophical arguments in support of rationing by life-years are remarkably wanting. We conclude by offering a fair alternative that adheres to the standard duties of beneficence, respect for persons, and justice.
Antiracist Praxis in Public Health: A Call for Ethical Reflections
First published: 11 April 2021
Abstract
The Covid-19 pandemic has revealed myriad social, economic, and health inequities that disproportionately burden populations that have been made medically or socially vulnerable. Inspired by state and local governments that declared racism a public health crisis or emergency, the Anti-Racism in Public Health Act of 2020 reflects a shifting paradigm in which racism is considered a social determinant of health. Indeed, health inequities fundamentally rooted in structural racism have been exacerbated by the Covid-19 pandemic, which calls for the integration of antiracist praxis to promote ethical public health research processes. This commentary describes ways in which antiracist praxis—which emphasizes empowerment of traditionally marginalized populations—offers strategies to explicitly address power imbalance, stigmatization, and other consequences of structural racism in public health research.
Employment-Based, For-Profit Health Care in a Pandemic
First published: 29 June 2020
Abstract
The emergence of Covid-19 in the United States has revealed a critical weakness in the health care system in the United States. The majority of people in the nation receive health care via employment-based health insurance from providers in a competitive market. However, neither employment-based health care nor a competitive health care market can adequately provide treatment during a global pandemic. Employment-based health care will fail to provide care for a large number of people in any destabilizing economic event, including a pandemic. Competitive for-profit health care systems distribute limited goods based on markets rather than health care needs. If a global pandemic results in unusually high demand for specific medical supplies, then these will be distributed suboptimally. The combined risk of suboptimal distribution of needed goods and a significant drop in health care access in a global pandemic indicates that the U.S. health care system has serious vulnerabilities that need to be addressed.
Disability Rights as a Necessary Framework for Crisis Standards of Care and the Future of Health Care
First published: 29 June 2020
Abstract
In this essay, we suggest practical ways to shift the framing of crisis standards of care toward disability justice. We elaborate on the vision statement provided in the 2010 Institute of Medicine (National Academy of Medicine) “Summary of Guidance for Establishing Crisis Standards of Care for Use in Disaster Situations,” which emphasizes fairness; equitable processes; community and provider engagement, education, and communication; and the rule of law. We argue that interpreting these elements through disability justice entails a commitment to both distributive and recognitive justice. The disability rights movement’s demand “Nothing about us, without us” requires substantive inclusion of disabled people in decision-making related to their interests, including in crisis planning before, during, and after a pandemic like Covid-19.
A Strategy to Prevent and Control Zoonoses?
First published: 29 June 2020
Abstract
The authors argue that in preventing and controlling the pandemic of Covid-19, we should have taken an offensive or proactive strategy rather than a defensive or reactionary one because the former type of approach can bring about more health benefits and fewer harms than can the latter. The offensive or proactive approach consists of two parts: The first part is to preemptively establish a barrier between a novel virus and humans in order to prevent the spillover of the virus into humans, and the second part is that, when a spillover fails to be prevented, we should take public interventions, such as contact tracing, social distancing, and quarantine and isolation, as early as when there are several dozens or one hundred or more cases that manifest symptoms with an unknown etiology in order to prevent an epidemic that is still limited to relatively small groups from developing into an outbreak.
Responding to Covid-19: How to Navigate a Public Health Emergency Legally and Ethically
First published: 26 March 2020
Abstract
Few novel or emerging infectious diseases have posed such vital ethical challenges so quickly and dramatically as the novel coronavirus SARS-CoV-2. The World Health Organization declared a public health emergency of international concern and recently classified Covid-19 as a worldwide pandemic. As of this writing, the epidemic has not yet peaked in the United States, but community transmission is widespread. President Trump declared a national emergency as fifty governors declared state emergencies. In the coming weeks, hospitals will become overrun, stretched to their capacities. When the health system becomes stretched beyond capacity, how can we ethically allocate scarce health goods and services? How can we ensure that marginalized populations can access the care they need? What ethical duties do we owe to vulnerable people separated from their families and communities? And how do we ethically and legally balance public health with civil liberties?
Fighting Novel Diseases amidst Humanitarian Crises
First published: 21 February 2019
Abstract
The Democratic Republic of the Congo is facing two crises: a potentially explosive Ebola epidemic and a major insurgency. But they are not wholly distinct from each other: the first is intertwined with the second, and public mistrust and political violence add a dangerous dimension to the Ebola epidemic. The World Health Organization and other health emergency responders will increasingly find themselves fighting outbreaks in insecure, misgoverned or ungoverned zones, possibly experiencing active conflict. Yet the WHO has neither the mission nor the capabilities to navigate these security threats. We cannot expect that the usual public health strategy will succeed when health workers’ lives are directly imperiled and community resistance runs deep. Tackling health emergencies amidst complex humanitarian crises requires fresh thinking. Here, we offer a blueprint for fighting diseases in complex humanitarian emergencies. The building blocks of security and trust include high-level political support, street-level diplomacy, community engagement, enhanced funding, and protection of health professionals working in conflict or disaster zones.
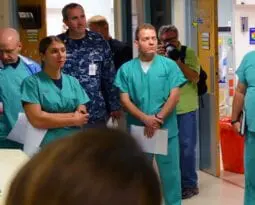
Emergency Nursing, Ebola, and Public Policy: The Contributions of Nursing to the Public Policy Conversation
First published: 21 September 2016
Abstract
Excellent patient care within the emergency department requires interdisciplinary training, teamwork, and communication to manage the chaos of the environment. Specifically, invasive procedures required to manage airway, breathing, and circulation via intubation, chest compressions, and establishing intravenous access can provide a direct benefit to save lives but also have the potential to harm both patients and health care clinicians alike; emergency health care clinicians can be exposed to significant amounts of blood and body fluids as well as other threats of physical and psychological harm. The ethical components of care in this environment are often under-recognized due to the need for rapid patient assessment and immediate action. Moreover, challenges to practice that can include lack of qualified personnel, equipment, and other resources to provide safe care to a large volume of patients can lead to moral distress in ED staff. Because the ED is a high-uncertainty, high-acuity environment, continuing interprofessional communication, collaboration, and planning is critical. Opportunities for multidisciplinary policy dialogue and the development of professional guidelines can make the ED a safer environment for both patients and providers.
Planning for Disaster
First published: 07 July 2015
Abstract
Some of my friends and relatives wonder why I want to spend my time thinking about social inequities in the context of natural disasters. I have tried to explain the importance of understanding how humanity’s responses mitigate or worsen the human toll of “acts of God.” Disaster ethics presents a unique set of challenges.
World Health Organization Reform: Lessons Learned from the Ebola Epidemic
First published: 04 March 2015
Abstract
It was October 2014, and Ebola was raging out of control in Guinea, Liberia, and Sierra Leone. Margaret Chan, the World Health Organization’s director-general, defended the organization against charges that its response was late and ineffective: “We are a technical agency, with governments having first priority to take care of their people.” In January 2015, the WHO executive board undertook a systematic reform of the agency’s performance, and Chan again offered a defense: I followed protocol, leaving it to the Africa office (AFRO) to respond. Yet the three nations could not possibly have stemmed the outbreak alone, and AFRO was known to be dysfunctional.
Ebola represents an inflection point requiring fundamental reform for the WHO. A failure of leadership will impact its status and legitimacy for a generation. Here, I offer five reforms that would transform it and ensure that it fulfills its constitutional mission as “the directing and coordinating authority on international health work.”
Ebola, Quarantine, and the Law
First published: 19 January 2015
Abstract
Judged by the key measures of morbidity and mortality, the United States has been very fortunate in the Ebola outbreak so far. We have had a limited number of cases and only a few fatalities. As of this writing, all of the health care workers who became infected in the United States have recovered, and none of the other nonhealth care contacts of Ebola patients has become infected. Yet by almost any other measure, the response to Ebola in the United States has been a disaster. Among other things, there has been a wealth of misinformation, politicization of public health, public panic, and unnecessary quarantine. There is plenty of blame to go around. But one often overlooked factor that complicated the response to Ebola is American public health law.
Public Health Emergencies: What Counts?
First published: 21 November 2014
Abstract
Although Jonathan Herington, Angus Dawson, and Heather Draper offer valuable insights on how to conceptualize health hazards and understand their effects on populations, I resist the label “public health emergency” for obesity, and here is why. It is important—politically and pragmatically—to be judicious with words that have legal and real-world consequences. Once a concept is stretched to encompass a broad swath of events, it loses its power. The broader the application of the term “public health emergency,” the more it loses the core idea of an emergent event. Thus, framing a long-simmering health hazard such as obesity as an emergency would mute the voices of public health authorities seeking a surge response to a truly emergent event, such as a rapidly spreading novel disease or a natural or human-made disaster.
What Counts? Justifications, Not Labels
First published: 04 March 2015
Abstract
A commentary on “Public Health Emergencies: What Counts?” by Lawrence O. Gostin, in the November-December 2014 issue.
In Case of Emergency: No Need for Consent
First published: January 1997
Abstract
The Food and Drug Administration (FDA) is amending its current informed consent regulations to permit harmonization of the Department of Health and Human Services’ (DHHS) policies on emergency research and to reduce confusion on when such research can proceed without obtaining an individual subject’s informed consent. This regulation provides a narrow exception to the requirement for obtaining and documenting informed consent from each human subject, or his or her legally authorized representative, prior to initiation of an experimental intervention. The exception would apply to a limited class of research activities involving human subjects who are in need of emergency medical intervention but who cannot give informed consent because of their life-threatening medical condition, and who do not have a legally authorized person to represent them. FDA is taking this action in response to growing concerns that current rules are making high quality acute care research activities difficult or impossible to carry out at a time when the need for such research is increasingly recognized.
From Hastings Center Bioethics Timeline:
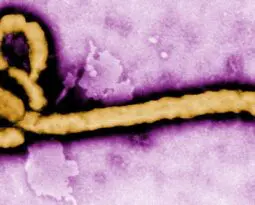
1976: Ebola Outbreak
In 1976, the first cases of Ebola virus were discovered near the Ebola River in Zaire (now known as the Democratic Republic of Congo). From the moment of its discovery until the present day, the disease has been a focus of controversy as narratives about scientific triumphalism conflicted with anthropological observations of cultural imperialism in the guise of science. Although indigenous cultural beliefs and practices were blamed for preventing effective treatment of the disease, a major cause of the virus’s spread turned out to be improper sterilization of needles, i.e., so-called scientific medicine. The outbreak was ultimately contained by traditional epidemiological methods of contact tracing, isolation, and quarantine.
https://www.sciencemag.org/news/2014/08/part-one-virologists-tale-africas-first-encounter-ebola
https://www.sciencemag.org/news/2014/08/part-two-virologists-tale-africas-first-encounter-ebola
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(14)62382-5/fulltext
1995: Outbreak. A Film from Warner Bros. Studios
Based on the book The Hot Zone by Richard Preston, the film is a plague narrative that depicts an outbreak in Africa of a highly infectious airborne virus. The movie brought to a wide audience the public health ethical issues that might arise from an Ebola-like virus.
https://www.warnerbros.com/movies/outbreak/
2019: Novel Coronavirus (SARS-CoV-2) Outbreak in Wuhan, China
The outbreak of the 2019 coronavirus disease (COVID-19) was first reported on December 31, 2019 in Wuhan China.
2020: Coronavirus (SARS-CoV-2) Pandemic
Massive outbreaks of Covid-19 (the illness caused by SARS-CoV-2) arise initially in China, rapidly becoming a pandemic, overwhelming health systems in Italy, Iran, Spain, and Brazil, as well as New York, California, Florida, Texas, Arizona, and many other countries, states, and cities. Resource shortages prompt development and implementation of plans for contingency and crisis standards of care. The latter were rarely implemented, despite apparent need, which forced consideration of public health ethics and ethically justifiable strategies to allocate scarce resources, such as ICU beds and mechanical ventilators, often focusing on the role of equity. Debates also arise around the relative value and costs of nonpharmaceutical interventions, especially “social distancing” measures such as masking, quarantine, and economic shutdowns. Extreme examples of racial, ethnic, and socioeconomic disparities in Covid-19 infection rates and outcomes are also reported. Though these disparities were not surprising given longstanding, well-documented underlying disparities in health care, they draw particular attention as they are reported at almost the same time as the emergence of widespread protests over racial injustice in policing, sparked by the murder of George Floyd.