Ethics and Pandemic Response
Selected resources from The Hastings Center.
Bioethics Briefings:
Pandemics: The Ethics of Mandatory and Voluntary Interventions
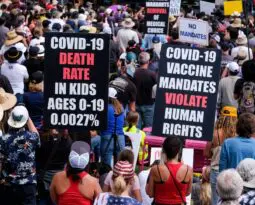
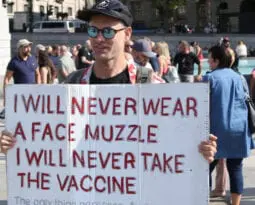
Nonpharmaceutical interventions (NPI) such as isolation and quarantine, school closures, and social distancing measures should be considered in the event of a pandemic, most notably during the COVID-19 pandemic. NPI work with the most benefit and least friction when they are voluntary, respect and rely on individual autonomy, and avoid the use of policy powers. Read our briefing to consider: What are the ethical implications of these interventions, particularly when it comes to balancing individual liberties with the need to protect the public’s health?
From Hastings Bioethics Forum:
- Covid is Surging. Most Young Children Are Still UnvaccinatedChildren are returning to classrooms amid another wave of Covid cases, but some public health leaders have leaned into the message that “most of us” can ignore the continued presence of Covid by taking just “a few basic steps,” such as staying up to date with vaccinations. “Most of us,” however, does not include families with young babies, among other groups for whom these steps are unavailable or insufficient.
- We Have Met the Enemy and It Is UsIn its early days, bioethics emphasized patient autonomy in the doctor-patient relationship. But patient autonomy is not the be-all and end-all principle to follow in all health care settings. Especially in lethal, airborne infectious disease pandemics.
- A Warning from China: After the Zero Covid PolicyA massive wave of Covid infections has begun now that China has ended much of its zero Covid policy. Three steps ought to be taken.
- Moving On from Covid? Immunocompromised People Can’tThe best case scenario for immunocompromised people like me would be universal masking in all public spaces. But I am willing to compromise.
- The CDC’s Misguided Medical Masking PolicyThe Center for Disease Control and Prevention’s revised guidelines have done away with universal masking at health care facilities, making masking optional if community Covid transmission isn’t high. It’s the latest attempt of public health officials to adapt their guidance to meet the country’s fatigued sensibilities. Some patients will be at risk.
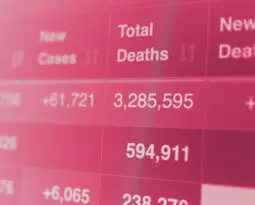
- How Many Covid-19 Deaths Should We Accept?President Biden recently declared that the Covid-19 “pandemic is over.” Some public health experts agreed with this assessment; others disagreed. What cannot be disputed is that nearly 12,000 Americans have died from Covid-19 over…
- Back to School: The Covid Vaccination ChoiceIt’s back-to-school season in the United States, the third one during the Covid pandemic, but the first in which all schoolchildren are eligible for Covid vaccines. Yet fewer than a third of children ages 5 to 11 are fully vaccinated, while the percentage of those under 5 who have started–let alone completed–vaccination is in the low single digits. Why? The answers are complicated.
- Treating Gun Violence as a Public Health Threat: Not Exactly What We MeantThis week, the United States saw two momentous public health events: one million deaths attributed to Covid and the 198th mass shooting of the year. Both the pandemic and gun shootings are threats to public health that are not being adequately addressed.
- California U-Turn on Vaccine Mandates for SchoolchildrenThe California legislature appears to have caved to pressure from opponents of a Covid vaccine mandate for schoolkids. I’d prefer to think of it as a wise and strategic retreat from a battle that mandate advocates could not win.
- Masks, Values, and a Lesson for Democracy?As mask mandates are rolled back and friends and neighbors debate the risks and benefits of masks and the merits or permissibility of mandating their use, we can catch a glimpse of the considerable extent to which values depend heavily on something other than pure reason. It’s a bit disappointing, perhaps. But it might be a useful lesson for democracy.
- Resilience and the Twin Medical Catastrophes of War and PandemicAs I sit here in my office at the Slovak Medical University in Bratislava, my colleagues are experiencing great moral anguish because of Russia’s invasion of neighboring Ukraine. Simultaneously, we are also confronting the Omicron wave of the Covid-19 pandemic. The war complicates and burdens health care here and in other border nations exponentially, and especially so in combination with the pandemic.
- I Was Never “Just” a VisitorCaregivers are not visitors. Hospital policies that restrict visits from family caregivers can harm patients.
- Global Health Justice: Now Is the TimeThe recognition of the social injustices surrounding the pandemic is an important opportunity to understand the longstanding links between health and social and global justice.
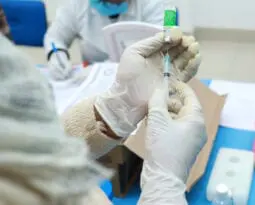
- Overcoming Covid Vaccine Hesitancy Among Minnesota’s Somali MuslimsWhen Covid-19 vaccines first became available last year, Somali Muslims in Minnesota–the largest Somali Muslim population in North America– were fearful and, consequently, their vaccination rate was low and their Covid-19 rate was high. But health professionals and community representatives worked together to understand and overcome their vaccine hesitancy.
- Another Pragmatic Public Health DecisionThere has been much criticism of the decision by the Centers for Disease Control and Prevention (CDC) to let Covid-infected people who are feeling better to stop quarantining after five days and simply wear a mask. But this sort of pragmatic decision has a long history in public health.
- With Pediatric Hospitalizations Rising, Reconsider Off-Label Covid Vaccination for Young ChildrenPfizer recently announced that its trials in children 2 to 5 years old produced a weaker than expected antibody response and that it would hold off requesting authorization from the Food and Drug Administration. This news creates opportunities – and additional challenges – for off-label use of Covid-19 vaccines in children,
- Should Clinicians Ask Hospitalized Covid Patients Why They Aren’t Vaccinated?The role of doctors, nurses and other clinicians is to treat patients without passing judgment and to fulfill their fiduciary duty. However, the Covid-19 pandemic has muddled these obligations.
- Vaccination Discrimination Goes Against Nursing EthicsSome health care providers are prioritizing patients who are fully vaccinated against Covid-19 over those who are unvaccinated. This is unethical.
- Studying Covid Vaccines in the Youngest KidsChildren have suffered both physical and mental illness during the pandemic. Nearly 200 children in the United States have died. Acute mental health crises increased during the pandemic. Getting children immunized is the best way to get back to normal. We suggest an option that would permit children under 5 to be vaccinated without waiting until traditional prospective randomized trials can be completed.
- Omicron, the Legacy of Renée Fox, and the Uncertain Practice of MedicineLike the pandemic, uncertainty, growing confidence, and the return of doubt come in waves. The Omicron variant is just the latest twist in this plot.
- Pathogens and HumansIn a 1988 essay on pandemics, Nobel laureate Joshua Lederberg wrote, “We have no guarantee that the natural evolutionary competition of viruses with the human species will always find ourselves the winner.”
- Is It Ethical to Prohibit Off-Label Use of Covid-19 Vaccines in Kids?In a new essay in the Hastings Center Report, we argue it is not. Yet the practice is prohibited.
- Vaccine Mandates for Kids: It’s Not Whether, But WhenStates and school boards around the country are engaged in a debate about whether to require middle and high school students to be fully vaccinated against Covid-19. The debate is not so much about whether to mandate. It’s when to do so.
- What Warrants Religious Exemption from Covid Vaccine Mandates?Faced with mandatory Covid vaccination, students and employees have appealed to religion as grounds for exemption. This latest conscience war within our culture wars presents a minefield of legal and philosophical complexities for states and health care systems.
- Who Will Be There to Care If There Are No More Nurses?The pandemic has laid bare the significant shortcomings of a health system rooted in an unsustainable financial model that exploits the physical and emotional labor of its nurses.
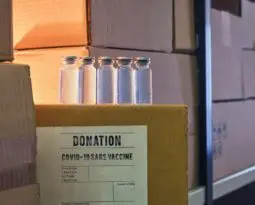
- Capitalist Philanthropy and Vaccine ImperialismThe commitments made by the wealthiest countries to share Covid vaccines and funding for international cooperation mechanisms are crucial, but insufficient. They reflect the “securitization of health,” a 21st century phenomenon whereby states turn health issues into national security issues.
- Public Reason, Public Schools, and Mask MandatesIn South Carolina, where I live, we are not just ignoring good arguments, but actually legislating on the basis of bad ones. The budget rule, Proviso 1.108, threatens the funding of schools that require masks.
- Love Thy Neighbor as Thyself: Building Community During CovidThe opposition to mask and vaccine mandates transcends the issue of individual liberty.
- Should Covid Vaccination Status Be Used to Make Triage Decisions?As the Covid-19 pandemic continues to strain health systems’ capacity to provide adequate care for critically ill patients, should patients’ vaccination status be considered in making triage decisions? This question sparked debate recently after the leak of an internal memo of the North Texas Mass Critical Care Guideline Task Force that proposed using patients’ Covid-19 vaccination status as a factor to assign intensive care beds.
- Fear of Doing Too Much Too Soon or Too Little Too Late: Research on Covid-19The Covid-19 pandemic has significantly affected the practice of clinical research. Researchers and IRBs have felt an urgency to respond more quickly than usual, aware that lives are at stake.
- Parents, Covid, and Trauma-Informed ChoicesAs the parent of a child under 5 years old, I am worried about what lies ahead for kids and Covid-19. The more contagious Delta variant is widely circulating, infecting kids at higher rates…
- The FDA and the Moral Distinction Between Killing and Letting DieWhy is the FDA dragging its feet in approving Covid vaccines for children under 12? Justifications lack moral weight.
- Vaccine Mandates for Health Care Workers Raise Several Ethical DilemmasThe moral justification for mandating covid vaccination for health care workers is clear. But what happens if some health care workers still refuse to be vaccinated, and there aren’t enough vaccinated staff to care for all the patients in a hospital?
- A Student’s Perspective: Universities Must Require VaccinationColleges and universities have an ethical obligation to mandate covid vaccines to protect the health and futures of both their students and the larger communities, in addition to promoting equality through education.
- Covid Doesn’t Justify Cutting Corners on Medical InterpretationMany hospitals are providing incomplete or subpar professional medical interpretation to the patients who need it–many of whom are disproportionately affected by Covid.
- Quality of Life? Suffering? Covid-19 Intensifies Challenges in Discussing Life-Sustaining TreatmentThe pandemic magnified the inherent difficulty and stress of conversations involving life-sustaining treatment by forcing clinicians and patients to engage in life-altering discussions via telephone and video conference, restricting nonverbal communication and eye contact, and eliminating the benefit of simply having another person nearby in time of crisis.
- Rugged American Individualism is a Myth, and It’s Killing UsThe American myth of rugged individualism, which often means “pulling yourself up by your own bootstraps,” is outdated, was never completely accurate. It is on full display during the coronavirus pandemic, contributing to cases and deaths.
- Covid Vaccine Patent Waivers are for Health SovereigntyThe United States, Russia, and China support temporary patent waivers for Covid vaccines. The waivers, which need support from other countries, would likely save lives in low- and middle-income countries.
- Instead of Vaccine Passports, Let’s Push for Global Justice in Vaccine AccessIn Costa Rica, where I live, only 24% of the population has received at least one vaccine dose because we have received very small amounts of vaccines. The Costa Rican president suggested that every person who can travel to the U.S. to get the jab, should do it. Vaccine tourism, then, seems to be another promising business opportunity for the powerful countries that have accumulated vaccines instead of redistributing them soon and fairly.
- Covid-19 in Argentina and the Abuse of BioethicsMany Latin American countries are being devastated by excessive loss of life from Covid-19, many sectors of society falling below the poverty line, and health systems being overwhelmed. As collateral damage, some countries in the region are witnessing an eruption of populism and autocratic trends and an increasing erosion of already weak and unstable democracies. Can bioethics be a useful tool for managing this crisis? Argentina provides a case study.
- C.D.C.’s Latest Mask Guidance: Science, Politics, and Public HealthThe C.D.C.’s latest policy guidance that people who have been fully vaccinated against the coronavirus virus no longer need to wear face masks indoors gets the science right, but policymaking wrong.
- Nope. A Covid-19 Travel Pass isn’t Just like the Yellow Card.Citing the Yellow Card as precedent for Covid-19 travel passes that exempt those with proof of vaccination from testing and quarantine mandates when crossing certain borders is an erroneous policy assumption that could prolong the pandemic and imperil global health.
- Should We Enroll Our Child in a Covid-19 Vaccine Trial?My partner and I are thinking a lot about this question. Moderna and Pfizer trials are running in our community–at the children’s hospital where I work as a clinical ethicist. The Pfizer trial began…
- After the Anniversary of Covid, Reckoning with Many New NormalsAnniversaries are complicated. In rehabilitation psychology, the anniversary of an accident that caused a brain or spinal cord injury can be a time for profound gratitude and for grief. Now that we have passed the one-year anniversary of the Covid pandemic, each of us continues to deal with the repercussions and wondering what the “new normal” may look like.
- Covid-19 Vaccine Hesitancy in Rural Communities? Checking Our AssumptionsAs access to vaccines increases, the popular press reports waning demand for vaccines in rural residents and points to vaccine hesitancy. But there may be other reasons why doses distributed to rural areas remain unclaimed.
- Exhortations to Trust Biomedical Experts: What’s Missing?Disagreements among biomedical experts regarding whether the scientific evidence supports delaying the second shot of Covid-19 vaccines or pausing the AstraZeneca and Johnson & Johnson vaccines because of very rare side effects bring to the fore missing aspects in exhortations to trust biomedical experts.
- Vaccinated and Still Isolated: The Ethics of Overprotecting Nursing Home ResidentsThe pandemic is not over, but light is beginning to crest the horizon. Vaccination rates, especially among older adults and their caregivers, are rising. As we begin to relax physical distancing requirements on restaurants…
- WHO-China Report on Covid: Important Step Forward, More to Be DoneThe World Health Organization recently released a long-anticipated report on SARS-CoV-2 origins, based on 28 days of field research and site visits in China conducted jointly by 17 international and WHO experts and 17…
- Too Taboo to Contemplate? Refusing Covid Vaccination for Some People with DementiaThere are a whole lot of us who think that, if we had dementia and were unable to live independently, we would prefer death. The idea that someone suffering from dementia and confined to a nursing home might actually welcome death is apparently so taboo that it cannot be openly contemplated.
- A Doctor Confronts the Burden of Judgment during the PandemicIs it wrong for doctors to judge their patients’ choices? I have reflected on this question while being on the frontline of the Covid-19 pandemic in New York City. Health care professionals are trained…
- Surrogate Decision-Making for Incarcerated Patients: A Pandemic-Inspired Call to ActionAs Covid-19 continues to plague the United States, insufficient attention has been paid to the role that incarcerated persons play in the persistence of this pandemic and the work that should be done to…
- Making Vaccine Appointments Is Tearing Us ApartThe Covid-19 vaccine rollout is currently a hub of individual, sociopolitical, and ethical activity. As we watch the numbers of daily doses administered rising, we may feel engaged in a successful, miraculous scientific project…
- How to Make It Right: Covid ReparationsReparations in various forms of compensation to the American victims of preventable Covid, who may experience lifelong health effects, is obligatory.
- Covid-19 Vaccination Certificates: Prospects and ProblemsNow, with limited distribution of vaccines with varying degrees of efficacy there is renewed interest in immunity passports; more accurately described as vaccination certificates. What remains to be determined is who may use this documentation for what purpose.
- Undocumented Immigrants and Covid-19 VaccinationWillingness to be vaccinated is not the only factor that may reduce vaccination rates. Fear is a powerful deterrent for individuals in hidden populations, especially undocumented immigrants. Even if their work or other circumstances place them at high risk of infection, many would be unlikely to risk the consequences of coming forward to be vaccinated.
- Working Around the System: Vaccine Navigators and Vaccine EquityVaccine navigators have emerged as a response to the complexity of mass vaccination for Covid-19.
- Why We Need a Covid-19 CommissionCongress recently announced plans for an independent commission to investigate the facts and causes of the January 6 insurrection at the U.S. Capitol. This 1/6 Commission is to be modelled after the 9/11 Commission. A national commission to investigate the disaster that the Covid-19 virus has caused in America must also be launched.
- Vaccine Hesitancy Is No Excuse for Systemic RacismFewer vaccines are going to Black people. While it’s easy to fall back on vaccine hesitancy as an excuse, systemic racism is to blame.
- Science in the Biden White House: Eric Lander, Alondra Nelson, and the Legacy of Lewis ThomasScience has replaced populism in the White House. For the first time, the president’s science advisor will be elevated to cabinet rank. There are other good omens, as well.
- Islamic Ethics, Covid-19 Vaccination, and the Concept of HarmVaccine hesitancy is a concern around the world, but negative attitudes among Muslims in particular toward some coronavirus vaccines have been the focus of attention in the media. Some scholars in Asia recently issued fatwa against the Chinese Covid-19 vaccine. Media coverage has characterized the Muslim world as a hotspot for vaccine hesitancy, but experts point out biases in this coverage and explain the underlying reasons.
- Should Covid Vaccination Schedules Deviate from the Status Quo–as a Last Resort?Last month, with concerns over the supply and coordinated administration of coronavirus vaccines escalating, the Centers for Disease Control and Prevention conceded that “any available mRNA COVID-19 vaccine” may be used to complete vaccination in “exceptional situations” preventing multi-dose manufacturer matching. While presented solely as a last resort, this guidance reflects a dilemma currently sweeping across the medical and health policy worlds: given limited supply, should vaccination efforts—still only authorized for emergency use in this country—deviate from evidence-driven, studied regimens to maximize individuals reached?
- Efficacy is Relative in a Public Health Crisis: Evaluating the Next Wave of Covid-19 VaccinesA third Covid vaccine candidate moving closer to potential FDA authorization is less effective than the two Covid vaccines already authorized in the United States. Is it ethical to offer a vaccine with lower efficacy? Is it ethical not to offer it in a public health emergency?
- Ethics Supports Seeking Population Immunity, Not Immunizing Priority GroupsVaccine allocation guidelines that prioritize people at greatest risk of Covid-19 require considerable administrative work (sometimes taking weeks). This is creating a bottleneck that has resulted in doses stuck in freezers not in arms. There’s a better, more ethical way to allocate vaccines.
- Surprising Surge of Egg Freezing during the Pandemic Raises Ethical QuestionsContrary to the expectations of many fertility clinics, demand for egg freezing has increased sharply during the Covid-19 pandemic, highlighting longstanding ethical concerns about egg freezing clinics.
- The Bioethics of Built Health Care SpacesAround the world, an alarming percentage of Covid-19 deaths occurred in long-term care facilities. Some of these deaths may have been avoided by changes in design. It’s time that bioethicists to take a closer look at the built health care environment.
- Masks Are Not Created EqualFinally, the Centers for Disease Control and Prevention is working on developing standards for masks to see which ones actually block viruses. In the meantime, though, we should all be acting on what we do know about the effectiveness of various masks against Covid.
- Ashamed to Be Vaccinated? The Ethics of Health Care Employees Forgoing Unfair PrioritySuppose you are young, healthy, employed in a health care system and that your line of work does not require leaving the low-risk comfort of your home. Now suppose that your employer offers you a vaccine. You know there are others in your community who are at greater risk of contracting and dying from Covid-19 than you. Should you accept the dose?
- Coronavirus Mutation PanicThe headlines are terrifying: A highly contagious new variant of the coronavirus is circulating in England. As the story spread, politicians and media outlets reported a devastating statistic: the new strain is 70% more transmissible than other strains of the virus. This has led to new lockdowns; many border closures; flight cancellations; and people fleeing the U.K. by train, boat, and plane. But is any of this necessary? Is the world suffering from mutation panic?
- Prioritizing the “1a”: Ethically Allocating Scarce Covid Vaccines to Health Care WorkersBeginning this week, guarded vehicles loaded with the first Covid-19 vaccine authorized in the United States are fanning out to hospitals across the country. In vaccine prioritization protocols health care workers, along with nursing home residents, make up phase “1a” – those who are first in line to be vaccinated. While much attention has been paid to who should come next, less is known about how hospitals are allocating vaccine doses among their staff. For many medical centers, the first shipments will only be enough to vaccinate a fraction of their workers. Who goes first within the “1a” category, and how are such decisions made?
- Global Allocation of Coronavirus VaccinesA Covid-19 vaccine developed by Pfizer and BioNTech has received emergency authorization in the United States and has been authorized in the countries, and a vaccine by Moderna is likely to be authorized soon. In spite of this good news, at least for the first couple of years, Covid-19 vaccines will be a scarce resource. Because low-income countries are likely to lose out in the scramble to get access to them, there have been calls for global solidarity. While equitable allocation of vaccines around the world would be ideal, it is unrealistic as a near-term goal.
- Bioethics, Nazi Analogies, and the Coronavirus PandemicThe year 2020 will be remembered as the first year of the coronavirus pandemic. But the pandemic was not alone in creating fear and dismay and raising ethical questions. Think of the rise in antisemitism, police violence against Black people, protests against immigration, and rallies by groups espousing Nazi slogans and symbols. Hate crimes, including murder, are the highest in years, according to the most recent FBI report, and were particularly aimed at Jews and Hispanics. Asian-Americans have been targeted as carriers of the so-called “China virus.”
- Resisting Public Health Measures, Then and NowOne of the most surprising aspects of the Covid-19 pandemic for those of us who teach the history of public health is how unwilling many Americans have been to adopt health measures to protect others. Over the Thanksgiving holiday, tens of millions of Americans traveled, despite the fact that the Centers for Disease Control and Prevention urged them to stay home and the overall death rate from the coronavirus is approaching 300,000. Should recent events make us revisit aspects of the history of public health? And how can these stories inform future public health efforts during pandemics?
- Human Plasma and Bioethics NationalismThe procurement of human plasma as a potential therapy for Covid-19 is one of the latest examples of bioethics nationalism, defined by Jonathan Moreno in this blog as “distinct bioethics standards [which] are formally proclaimed as a matter of right by a sovereign state.” The race for a Covid cure pushes at the weak seams in the international liberal order in much the same way that Covid appears to be pushing at health care systems.
- Ethics of Emergency Use Authorization During the PandemicThe Food and Drug Administration’s rigorous guidance for an emergency use authorization of a Covid vaccine was met by resistance from the White House, since some of the terms would make it virtually impossible to issue a vaccine-related emergency authorization before Election Day. Understanding the ethical dimensions of issuing it for a vaccine can provide clarity on the necessity of the FDA’s stringent guidelines.
- Ethics of Placebo Controls in Coronavirus Vaccine TrialsMultiple candidate vaccines for coronavirus are being evaluated scientifically in a process of unprecedented speed, and thousands of individuals around the world have volunteered to participate in placebo-controlled phase III field trials. If, or when, one of these candidate vaccines is proved to be safe and effective and receives an emergency use authorization by the Food and Drug Administration, will it continue to be ethical to enroll participants in other coronavirus trials that randomize half of them to a placebo?
- Amid the Pandemic and Racial Injustice, Greater Empathy in Medical SchoolEmpathy does not need to dissipate as we endure medical training. Both the pandemic and the national reckoning over racial injustice and police brutality have touched every aspect of life as we know it, and medical training and education have been no exception.
- Could the Common Cold Help Stop Covid-19? We Need to Know–Now.In an essay published in Scientific American, we call for immediate and intensive research into the possibility that exposure to one of the coronaviruses that cause the common cold could decrease the severity of Covid-19, and could be leveraged to expand what’s been called “pre-existing” immunity to the disease by deliberate transmission of common cold coronaviruses. Here, we expand on our proposal.
- Volunteering for a Covid Vaccine Trial: Fulfilling Hindu Obligations or Fostering Pharmaceutical Company Profits?Volunteering for a Covid-19 vaccine trial satisfied my altruistic goals and harmonizes with my Hindu beliefs. But I am troubled that a drug company is going to profit from my altruism and my religious obligations.
- Living through the Pandemic in New ZealandIn New Zealand we have been saved from the worst devastations of Covid-19 by a firm government, courage and care for one another, and our geographic “moat.” With the recent minor surge of cases, our government has, once again, encouraged us to respond as a team of 5 million. We have been guided by the slogan “Be kind.”
- Fair Compensation for Rare Vaccine HarmsAs multiple Covid vaccine candidates enter clinical trials and hopefully move closer to approval, one important unanswered question is how to compensate the rare cases of serious vaccine harm.
- We Can’t Forget the Nation’s Other EpidemicCovid isn’t merely overshadowing the drug overdose crisis—it’s directly worsening it.
- Are Physicians Hypocrites for Supporting Black Lives Matter Protests and Opposing Anti-Lockdown Protests? An Ethical AnalysisPhysicians have been vocal in condemning the anti-lockdown protests while endorsing and even participating in the Black Lives Matter protests. This has led to criticism of the medical community for being inconsistent and hypocritical. What does an ethical analysis reveal?
- Covid-19 and Deafness: Why the Protocols Fall ShortI am hard-of-hearing; I wear two hearing aids, and Covid-19 has made all forms of human interaction extraordinarily difficult.
- Did Russia’s Most Influential Bioethicist Get a Coronavirus Vaccine?Along with the announcement that his government had approved Sputnik V, the supposed Russian coronavirus vaccine, Vladimir Putin also indulged in a moment of paternal pride: Wanting to confirm his personal confidence in the vaccine, he mentioned that one of his daughters was among the early recipients. This raises a couple of intriguing questions: Which daughter was it? And why does it matter?
- Hacking Ventilators in a PandemicThe Covid-19 pandemic continues to test and occasionally overwhelm health care institutions. Many practitioners may face the ethically challenging scenario of having to ration ventilators while triaging patients in “crisis care.” Ventilator shortages have led to innovative ventilator design “hacks.” Are these improvised ventilators ethical?
- Is the Coronavirus Pandemic Accelerating Bioethics Nationalism?The global crisis created by the coronavirus pandemic and the rush to create and distribute a vaccine widely hoped to be a “silver bullet” that can facilitate a return to “normalcy” threatens to upend seven decades of assumptions about bioethical norms.
- Against Personal Ventilator ReallocationPersonal ventilators used by people with disabilities should not reallocated to people with Covid-19. Triage protocols should be immediately clarified and explicitly state that personal ventilators will be protected in all cases.
- Lawsuits of Last Resort: Employees Fight for Safe Workplaces during Covid-19As more workplaces open up, a seldom-used legal action is being taken against employers charged with inadequately protecting employees from the coronavirus: public nuisance lawsuits.
- The Americans with Disabilities Act at 30: A Cause for Celebration During Covid-19?A central mandate of the ADA is to make the goods of society accessible to people with disabilities and overcome their segregation in civil society through reasonable accommodation that allows them to go to work, live with their neighbors, and avoid institutionalization. But let’s not delude ourselves with historic sentimentality as disability law is placed under tremendous stress by the pandemic.
- On Being a Foster Parent During CovidI knew that being a foster parent would be demanding, but I was unprepared for the extent of the challenges, which were exacerbated by the pandemic.
- Pandemic Language
- Before We Turn to Digital Contact Tracing for Covid, Remember Surveillance in the SixtiesIs it unrealistic to believe that phone apps for digital Covid contact tracing can be designed and regulated in ways that prevent the information they collect from being misused? It’s worth remembering surveillance of Vietnam War protesters and Martin Luther King Jr.
- Covid-19 Makes Clear that Bioethics Must Confront Health DisparitiesWith some reluctance, I’ve come to the sad realization the COVID-19 pandemic has been a stress test for bioethics, a field of study that intersects medicine, law, the humanities and the social sciences. As both a physician and medical ethicist, I arrived at this conclusion after spending months at what was once the epicenter of the pandemic: New York City. I was overseeing a 24/7 bioethics consultation service.
- Using the Pandemic as an Excuse to Limit AbortionSeveral states, including Ohio, Alabama, Arkansas, Texas, Iowa, and Oklahoma, declared abortion a nonessential service at some point during the pandemic, meaning that it was effectively banned until the crisis passed. Supporters of the policies maintain that abortion is an elective procedure whose medical resources are better off used in the fight against the pandemic. But abortion opponents have been taking advantage of the current circumstances to limit abortion access.
- Social-Change Games Can Help Us Understand the Public Health Choices We FaceBefore there was the Covid-19 pandemic, there was Pandemic. This tabletop game, in which players collaborate to fight disease outbreaks, debuted in 2007. Expansions feature weaponized pathogens, historic pandemics, zoonotic diseases, and vaccine development races. Game mechanics modelled on pandemic vectors provide multiple narratives: battle, quest, detection, discovery. There is satisfaction in playing “against” disease–and winning. Real pandemic is not as tidy as a game. But can games support understanding about the societal challenges we now face? Yes.
- Accepting the Challenge: Covid Vaccine Challenge Trials Can Be Ethically JustifiedThe Covid-19 pandemic is unlikely to end until there is a safe, effective, and widely distributed vaccine. How soon can researchers achieve this goal? The answer largely depends on which strategies researchers are willing to adopt. One potential strategy is to conduct human challenge studies, in which researchers give an experimental vaccine to healthy volunteers and then test—or “challenge”—the vaccine by purposely exposing volunteers to the virus. Although a growing number of voices are calling on researchers to employ this strategy, the proposal is generating a heated debate about the ethics of such research.
- Cracks in the System: Lessons Learned from the Covid-19 PandemicThe United States leads the world in coronavirus cases and deaths. Although many people have called out the inadequacies of our health care system, Covid-19 has exposed the most significant shortcomings. The need for change can no longer be ignored. Here are three lessons from this pandemic that should be leveraged for change.
- “If the virus doesn’t kill us, the stress and anxiety will.” Immigrants during CovidGrowing isolation, financial challenges and disease burden during the Covid-19 pandemic threaten to worsen the mental health needs of the entire U.S. population. These challenges are heightened among immigrants with untreated chronic mental health conditions as they experience added psychological distress owing to harsh immigration policies and worsening structural barriers to health during the pandemic.
- Bringing Ethics into the Global Coronavirus ResponseCovid-19 is a matter of public and global health ethics, and the pandemic is currently accelerating cooperation within and contributions from these fields. A meeting on June 27, hosted by the European Union and Global Citizen, is the latest example another global pledging event on June 27, will include governments and large institutions, as well as individuals and communities worldwide.
- After the Surge: Prioritizing the Backlog of Delayed Hospital ProceduresThe rewards of social distancing are beginning to accrue in former hotspots such as Seattle, the New York metropolitan area, and the San Francisco Bay Area, where the number of new Covid-19 cases requiring hospitalization is declining. Assuming the rewards hold in the face of pressures to reopen the economy, hospitals will now face challenges of reopening their own nonpandemic services for patients whose elective surgeries and other procedures were postponed. Which patients should get priority?
From Hastings Center Report:
Expanding Paid Sick Leave Laws: The Public Health Imperative
First published: 24 February 2023
Abstract
A key public health measure has received far too little attention over the course of the Covid-19 pandemic: paid sick leave policies that encourage people at risk of spreading disease to stay home rather than come to work. The United States is one of the only developed countries that fails to guarantee paid sick leave at the federal level, leaving a patchwork of state and private policies that undersupply time off when people are contagious and protect top wage earners at wildly disproportionate rates compared with what workers with lower incomes experience. Other countries have shown that sick leave mandates are neither unjustified burdens on employers nor gratuitous giveaways to employees. In fact, sick leave saves on health care costs by making employees less likely to infect coworkers, to be absent for longer themselves, or to need treatment in expensive hospital emergency departments. Nationally guaranteed sick leave is urgently needed to promote public health.
Covid-19, Free Exercise, and the Changing Constitution
First published: 16 November 2021
Abstract
The Covid-19 pandemic has brought bioethics back to five topics—justice, autonomy, expert authority, religion, and judicial decisions—that were central during its formative period but has cast a new light on each, while also tangling public health policy in the current, rather radical, reshaping of the role of organized religion in society.
In This Together: Navigating Ethical Challenges Posed by Family Clustering during the Covid-19 Pandemic
First published: 11 April 2021
Abstract
Harrowing stories reported in the media describe Covid-19 ravaging through families. This essay reports professional experiences of this phenomenon, family clustering, as encountered during the pandemic’s spread across Southern California. We identify three ethical challenges following from it: Family clustering impedes shared decision-making by reducing available surrogate decision-makers for incapacitated patients, increases the emotional burdens of surrogate decision-makers, and exacerbates health disparities for and the suffering of people of color at increased likelihood of experiencing family clustering. We propose that, in response to these challenges, efforts in advance care planning be expanded, emotional support offered to surrogates and family members be increased, more robust state guidance be issued on ethical decision-making for unrepresented patients, ethics consultation be increased in the setting of conflict following from family clustering dynamics, and health care professionals pay more attention to systemic and personal racial biases and inequities that affect patient care and the surrogate experience.
When Following the Rules Feels Wrong
First published: 25 February 2021
Abstract
The Covid-19 pandemic has created a clinical environment in which health care practitioners are experiencing moral distress in numerous and novel ways. In this narrative reflection, a pediatric palliative care physician explores how his hospital’s strict visitation policy set the stage for moral distress when, in the early months of the pandemic, it prevented two parents from being together at the bedside of their dying child.
Patients Left Behind: Ethical Challenges in Caring for Indirect Victims of the Covid-19 Pandemic
First published: 28 August 2020
Abstract
In response to the Covid-19 pandemic, health care systems worldwide canceled or delayed elective surgeries, outpatient procedures, and clinic appointments. Although such measures may have been necessary to preserve medical resources and to prevent potential exposures early in the pandemic, moving forward, the indirect effects of such an extensive medical shutdown must not outweigh the direct harms of Covid-19. In this essay, we argue for the reopening of evidence-based health care with assurance provided to patients about the safety and necessity of high-value vaccinations, screenings, therapeutics, and procedures. To ensure that virtually all non-Covid-related services do not come to a halt again, health care systems and physician practices must preemptively increase their capacity, secure adequate personal protective equipment to safeguard health care personnel, and develop a measured approach to reclosing such routine health care, should it become necessary in the future.
The Ethics of Everyday Life in the Midst of a Pandemic
First published: 29 June 2020
Abstract
Elderly individuals are at higher risk of serious illness and death if they become infected by the coronavirus. During the current pandemic, my wife and I, at ages seventy-two and seventy-one, respectively, have been paying a person laid off from a job to purchase groceries—a practice that exposes the shopper to risk of infection for our benefit. In this essay, I examine this practice with respect to the normative concepts of treating another person as a means, coercion, exploitation, and complicity.
Walls
First published: 29 June 2020
Abstract
In a field that strives to care for patients and families together, what can palliative care clinicians do when patients’ families are physically absent? The Covid-19 pandemic has put both literal and figurative walls between health care professionals and families. How health care workers respond to these disconnections might have a lasting impact on patients, on families, and on our practice. Recently, I saw this in the case of a patient our palliative care team was consulted to see. Mr. B was minimally responsive and dying from multisystem organ failure of unclear etiology. As in other cases during this pandemic, our team became a facilitator of interaction between the patient and the physically absent family, seeing an intimacy we normally would not, in this case, by being present while our intern held the phone to Mr. B’s ear for an end-of-life call from his wife, son, and daughter. Such moments force us clinicians to be even more present for our families and patients, and they allow us to bear witness to the strength and sadness and love that we might otherwise miss.
Digital Contact Tracing, Privacy, and Public Health
First published: 29 June 2020
Abstract
Digital contact tracing, in combination with widespread testing, has been a focal point for many plans to “reopen” economies while containing the spread of Covid-19. Most digital contact tracing projects in the United States and Europe have prioritized privacy protections in the form of local storage of data on smartphones and the deidentification of information. However, in the prioritization of privacy in this narrow form, there is not sufficient attention given to weighing ethical trade-offs within the context of a public health pandemic or to the need to evaluate safety and effectiveness of software-based technology applied to public health.
A Strategy to Prevent and Control Zoonoses?
First published: 29 June 2020
Abstract
The authors argue that in preventing and controlling the pandemic of Covid-19, we should have taken an offensive or proactive strategy rather than a defensive or reactionary one because the former type of approach can bring about more health benefits and fewer harms than can the latter. The offensive or proactive approach consists of two parts: The first part is to preemptively establish a barrier between a novel virus and humans in order to prevent the spillover of the virus into humans, and the second part is that, when a spillover fails to be prevented, we should take public interventions, such as contact tracing, social distancing, and quarantine and isolation, as early as when there are several dozens or one hundred or more cases that manifest symptoms with an unknown etiology in order to prevent an epidemic that is still limited to relatively small groups from developing into an outbreak.
Should Institutions Disclose the Names of Employees with Covid-19?
First published: 12 April 2020
Abstract
Prestigious University is a large, private educational institution with a medical school, a university hospital, a law school, and graduate and undergraduate colleges all on a single campus. In the face of the Covid-19 pandemic, students were told during spring break to return to campus only briefly to retrieve their belongings. Classes then went online. On March 23, 2020, the faculty, students, and staff were emailed the following by the university’s director of infection control and public health:
We have become aware that a Prestigious University staff member has tested positive for the virus that causes Covid-19. The individual, who was last on campus on March 16, is now in isolation at their permanent residence and is doing well clinically. The university has already identified those members of our community who may have been in close contact with this individual, and we are working to notify them. Further, this individual’s local health department has a protocol for identifying people who have been in direct contact with anyone testing positive for Covid-19 (such as this Prestigious University staff member) so that they can self-quarantine and watch for COVID-19 symptoms for a period of 14 days from their last contact with the infected individual.
A professor in the Philosophy Department has asked the ethicists at the medical school whether such contact tracing suffices. “Don’t the members of the community deserve to know who this is? Isn’t there a mandate to identify this person in order to maximize public health benefits and slow the spread of this deadly virus?”
Responding to Covid-19: How to Navigate a Public Health Emergency Legally and Ethically
First published: 26 March 2020
Abstract
Few novel or emerging infectious diseases have posed such vital ethical challenges so quickly and dramatically as the novel coronavirus SARS-CoV-2. The World Health Organization declared a public health emergency of international concern and recently classified Covid-19 as a worldwide pandemic. As of this writing, the epidemic has not yet peaked in the United States, but community transmission is widespread. President Trump declared a national emergency as fifty governors declared state emergencies. In the coming weeks, hospitals will become overrun, stretched to their capacities. When the health system becomes stretched beyond capacity, how can we ethically allocate scarce health goods and services? How can we ensure that marginalized populations can access the care they need? What ethical duties do we owe to vulnerable people separated from their families and communities? And how do we ethically and legally balance public health with civil liberties?
Quarantine Controversy: Kaci Hickox v. Governor Chris Christie
First published: 06 May 2016
Abstract
Nurse Kaci Hickox is among the “Ebola Fighters” honored by Time magazine as its 2014 Person of the Year, having treated Ebola patients in Sierra Leone while volunteering with Médecins Sans Frontieres. When she returned to the United States in October 2014, she was quarantined in New Jersey for three days before returning home to Maine under the terms of a negotiated release. A year later, in October 2015, Hickox filed suit in federal court against Governor Chris Christie and New Jersey health officials, claiming that the quarantine violated her civil rights. Her complaint asserts that New Jersey officials lacked the authority to quarantine her because she did not pose a significant risk of transmission. The lawsuit raises important questions about disease-transmission risk, the inability of science to rule out certain theoretical risks, and the state’s power to quarantine. It also demonstrates that population health depends on respecting individual liberty and using the best available epidemiological data to set public health policy.
Ebola, Quarantine, and the Law
First published: 19 January 2015
Abstract
Judged by the key measures of morbidity and mortality, the United States has been very fortunate in the Ebola outbreak so far. We have had a limited number of cases and only a few fatalities. As of this writing, all of the health care workers who became infected in the United States have recovered, and none of the other nonhealth care contacts of Ebola patients has become infected. Yet by almost any other measure, the response to Ebola in the United States has been a disaster. Among other things, there has been a wealth of misinformation, politicization of public health, public panic, and unnecessary quarantine. There is plenty of blame to go around. But one often overlooked factor that complicated the response to Ebola is American public health law.
From Hastings Center Bioethics Timeline
1976: Ebola Outbreak
In 1976, the first cases of Ebola virus were discovered near the Ebola River in Zaire (now known as the Democratic Republic of Congo). From the moment of its discovery until the present day, the disease has been a focus of controversy as narratives about scientific triumphalism conflicted with anthropological observations of cultural imperialism in the guise of science. Although indigenous cultural beliefs and practices were blamed for preventing effective treatment of the disease, a major cause of the virus’s spread turned out to be improper sterilization of needles, i.e., so-called scientific medicine. The outbreak was ultimately contained by traditional epidemiological methods of contact tracing, isolation, and quarantine.
https://www.sciencemag.org/news/2014/08/part-one-virologists-tale-africas-first-encounter-ebola
https://www.sciencemag.org/news/2014/08/part-two-virologists-tale-africas-first-encounter-ebola
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(14)62382-5/fulltext
1995: Outbreak. A Film from Warner Bros. Studios.
Based on the book The Hot Zone by Richard Preston, the film is a plague narrative that depicts an outbreak in Africa of a highly infectious airborne virus. The movie brought to a wide audience the public health ethical issues that might arise from an Ebola-like virus.
https://www.warnerbros.com/movies/outbreak/
2019: Novel Coronavirus (SARS-CoV-2) Outbreak in Wuhan, China
The outbreak of the 2019 coronavirus disease (COVID-19) was first reported on December 31, 2019 in Wuhan China.
2020: Coronavirus (SARS-CoV-2) Pandemic
Massive outbreaks of Covid-19 (the illness caused by SARS-CoV-2) arise initially in China, rapidly becoming a pandemic, overwhelming health systems in Italy, Iran, Spain, and Brazil, as well as New York, California, Florida, Texas, Arizona, and many other countries, states, and cities. Resource shortages prompt development and implementation of plans for contingency and crisis standards of care. The latter were rarely implemented, despite apparent need, which forced consideration of public health ethics and ethically justifiable strategies to allocate scarce resources, such as ICU beds and mechanical ventilators, often focusing on the role of equity. Debates also arise around the relative value and costs of nonpharmaceutical interventions, especially “social distancing” measures such as masking, quarantine, and economic shutdowns. Extreme examples of racial, ethnic, and socioeconomic disparities in Covid-19 infection rates and outcomes are also reported. Though these disparities were not surprising given longstanding, well-documented underlying disparities in health care, they draw particular attention as they are reported at almost the same time as the emergence of widespread protests over racial injustice in policing, sparked by the murder of George Floyd (see below).