Bioethics Forum Essay
Studying Covid Vaccines in the Youngest Kids
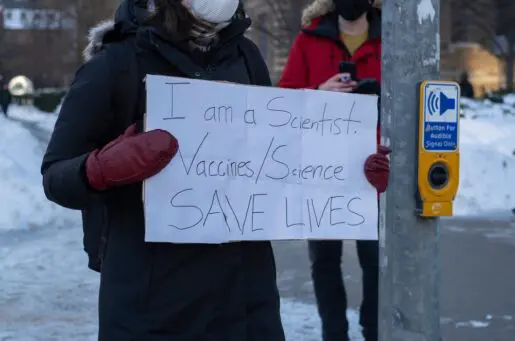
Children have suffered both physical and mental illness during the pandemic. Nearly 200 children in the United States have died. Acute mental health crises increased during the pandemic. Getting children immunized is the best way to get back to normal.
But Covid vaccines are not approved for children under 5 years old. Studies of vaccine safety and efficacy in this age group are under way. But emergency use authorization (EUA) of a Covid vaccine for the youngest children isn’t expected until next summer. Ordinarily, a vaccine that was approved for older children and teens might be used off-label in younger children. But off-label use of Covid vaccines is not permitted. This restriction is unusual, note Elizabeth Lanphier and Shannon Fyfe in a recent essay in which they also argue that the prohibition is unethical. Most drugs that are approved for adults can be used off-label in children if pediatricians believe that they would be safe and effective.
We suggest an alternative to off-label use that would permit children under 5 to be vaccinated without waiting until traditional prospective randomized trials can be completed. The option is to conduct open-label, non-randomized comparison studies. This is a study design that has been used in other domains, such as HIV research and care of diabetes complications. Parents could choose whether their child got a vaccine or a placebo. Both groups would be followed for outcomes. Open-label studies would allow a comparison group to the vaccinated children and an estimation of the safety and efficacy of the vaccine.
Such trials would not be as scientifically rigorous as a traditional study since randomization minimizes the effects of confounding factors that are known to influence the outcome, such as wearing masks and other preventive measures. But the studies would generate more information than off-label use of vaccines that haven’t been studied in young children. Open-label trials are fairly common, particularly when the benefits of the drug under study are such that giving a placebo would be unethical but there is still a need to gain knowledge about long-term safety and/or efficacy.
Why choose this option? Given that state of knowledge and politics about Covid-19 vaccines, it is likely that most parents have strong opinions about whether or not they want to vaccinate their children. In one study of parents of children ages 5 to 11, only about a third of the parents strongly preferred that their child receive the vaccine, about a third were hesitant, and a quarter were strongly opposed. Only 4% were willing to enroll their child in a randomized trial.
Parents who are hesitant about vaccines or participation in research are unlikely to enroll their children in a trial. Parents who are eager to have their children vaccinated may find the possibility of randomization into the placebo arm too risky and prefer to take their chances and wait for an EUA or even full approval.
Traditional randomized trials of Covid-19 vaccines in children under 5 years of age will likely be completed soon. But they will have small numbers of patients and will not be powered to find rare adverse reactions. A larger, open-label trial would provide more evidence about safety and efficacy. Such evidence might help overcome some portion of vaccine hesitancy. It would probably be easier to enroll children in an open-label, parent-choice study that would allow comparison in outcomes between the vaccinated and unvaccinated children than it would be to enroll children in a traditional blinded, randomized trial. An open-label trial would be limited by lack of randomization and all the questions that would arise about whether other infection-preventing behaviors were different in the two groups. But it would be better than nothing.
As with most bioethical dilemmas, all the choices are problematic. But a choice must be made. Children in the U.S. are suffering harms due to the pandemic mitigation strategies and ongoing pandemic hospital surges. Immunization would lead to reduction in those harms. Some parents strongly believe that. Some parents don’t. This unique social situation demands a broader assessment of the ethics and feasibility of researching vaccines for emergency use.
Once an EUA has been issued, the vaccine would no longer be off-label, but initiating an open-label trial at that time would continue to gather important data. A large open-label parent choice trial, concurrent with or after the current traditional studies, would be a good compromise between access to a vaccine that protects against Covid and protection against potential vaccine side effects for young children in the U.S.
Ian D. Wolfe, PhD, RN, (@iandwolfe) is a clinical ethicist at Children’s Minnesota. John D. Lantos, MD, (@johnlantos) is director of Children’s Mercy Bioethics Center at Children’s Mercy Kansas City, a professor of pediatrics, and a Hastings Center fellow.