Bioethics Forum Essay
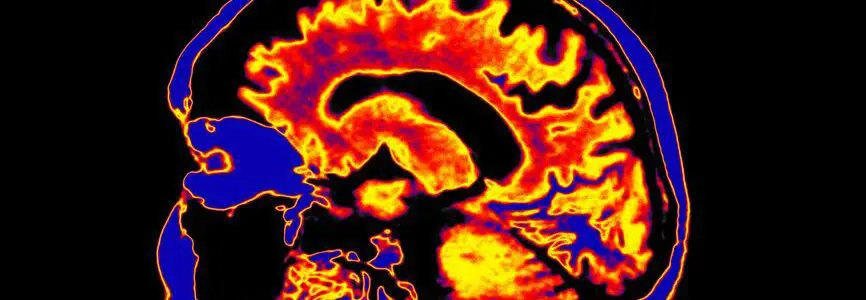
Proposal for Revising the Uniform Determination of Death Act
Organ transplantation has saved many lives in the past half-century, and the majority of postmortem organ donations have occurred after a declaration of death by neurological criteria, or brain death. However, inconsistencies between the biological concept of death and the diagnostic protocols used to determine brain death–as well as questions about the underlying assumptions of brain death–have led to a justified reassessment of the legal standard of death. We believe that the concept of brain death, though flawed in its present application, can be preserved and promoted as a pathway to organ donation, but only after particular changes are made in the medical criteria for its diagnosis. These changes should precede changes in the Uniform Determination of Death Act (UDDA).
The UDDA, approved in 1981, provides a legal definition of death, which has been adopted in some form by all 50 states. It says that death can be defined as the irreversible cessation of circulatory and respiratory functions or of brain functions. The act defines brain death as “irreversible cessation of all functions of the entire brain, including the brainstem.” This description is based on a widely held assumption at the time that the brain is the master integrator of the body, such that when it ceases to function, the body would no longer be able to maintain integrated functions. It was presumed that this would result in both cardiac and pulmonary arrest and the death of the body as a whole. Now that assumption has been called into question by exceptional cases of individuals on ventilators who were declared brain dead but who continued to have function in the hypothalamus.
A new committee of the Uniform Law Commission will study the need for and feasibility of updating the Uniform Determination of Death Act. “Issues to be considered include lack of uniformity in the medical standards used to determine death by neurologic criteria, the relevance of hormonal functions [and] whether notice should be provided before a determination of death,” said Samuel Thumma, the committee’s chair. He also said that the committee is considering whether consent should be required before brain death diagnostic testing can be conducted.
One proposed revision being considered is the Revised Uniform Determination of Death Act (RUDDA), published by Ariane Lewis, Richard J. Bonnie, and Thaddeus Pope. It would specify that American Academy of Neurology guidelines would constitute the legally mandated “medical standard” of brain death and would exclude hypothalamic function from those brain functions that must be tested. The currently accepted medical standards for a brain death diagnosis do not test for cessation of hypothalamic hormonal or homeostatic function. This could be interpreted as inconsistent with the statutory requirements for declaration of death, “all functions of the entire brain,” (emphasis added) if they were seen to require considering the pituitary and hypothalamus as part of the entire brain. The RUDDA proposal would also authorize brain death determinations, including apnea tests, without consent, because those authors do not believe that families should have the legal authority to veto these medical evaluations.
A subsequent response, authored by D. Alan Shewmon and co-signed by over 100 bioethicists, agrees that the UDDA needs revision, but considers the proposed RUDDA approach wrongheaded. (A Hastings Bioethics Forum essay summarized the alternative proposal.) Despite their having a wide variety of perspectives on the issue, these co-authors came to consensus on the following points:
- The adult and pediatric diagnostic guidelines for brain death have a nonnegligible risk of false positive error—declaring a living person dead.
- Hypothalamic function is more relevant to the organism as a whole than any brainstem reflex. It may persist when reflexes are absent in patients declared brain dead.
- The apnea test carries a risk of precipitating brain death in a patient who is not dead, provides no benefit to the patient, does not reliably accomplish its intended purpose as a definitive and indispensable marker of brain death, and is not even absolutely necessary for diagnosing brain death per the American Academy of Neurology guidelines. At the very least, informed consent should be required before conducting an apnea test, as it is before many procedures that are much more beneficial and less risky.
- Objections to a neurologic criterion of death are not based only on religious belief, or ignorance. People have a right to not have a concept of death that experts vigorously debate imposed upon them against their judgment and conscience. Any revision of the UDDA should therefore contain an opt-out clause for those who accept only a circulatory-respiratory criterion.
Although we are not in perfect alignment with Shewmon et al, the undersigned bioethicists of Georgetown University affirm our general agreement with their statement and reject the RUDDA as proposed by Lewis et al. We furthermore assert the following:
The concept of brain death remains defensible as an instance of the brain ceasing to act as an essential, integrating, and life-preserving organ. Brain death, then, is “a single event, consisting in the total disintegration of that unitary and integrated whole that is the personal self. It results from the separation of the life principle (or soul) from the corporeal reality of the person.” However, the criteria for determining brain death under current diagnostic guidelines are inadequate or insufficient. Problems with the criteria are demonstrated by well-documented cases of “chronic brain death”: pregnant women declared brain dead who were maintained on ventilators for weeks until the fetus was viable, and children such as Jahi McMath, who was maintained on a ventilator for years, growing and even entering puberty. Moreover, current criteria for brain death are often misapplied in clinical settings. In fact, the American Academy of Neurology has recognized:
severe limitations in the current evidence base. Indeed, there is only one study that prospectively derived criteria for the determination of brain death. Despite the paucity of evidence, much of the framework necessary for the development of “accepted medical standards” for the declaration of brain death is based on straightforward principles. These principles can be derived from the definition of brain death provided by the Uniform Determination of Death Act (UDDA). To determine “cessation of all functions of the entire brain, including the brain stem,” physicians must determine the presence of unresponsive coma, the absence of brainstem reflexes, and the absence of respiratory drive after a CO2 challenge. To ensure that the cessation of brain function is “irreversible,” physicians must determine the cause of coma, exclude mimicking medical conditions, and observe the patient for a period of time to exclude the possibility of recovery. The UDDA-derived principles define the essential elements needed to determine brain death. However, because of the deficiencies in the evidence base, clinicians must exercise considerable judgment when applying the criteria in specific circumstances. (emphasis added)
Revision of the UDDA should first defer to a revision of the guidelines. Clinical criteria for the diagnosis of “cessation of all functions of the entire brain” must include all pertinent functions, including hypothalamic functions such as hormone release and regulation of temperature and blood pressure, to avoid the specter of neurologic recovery in those who fulfill the current clinical criteria for the diagnosis of brain death.
It is likely that the failure to account for a full set of pertinent brain functions has led to inconsistent diagnoses and conflicting results. Such inconsistencies, although well-documented in a number of cases, may have been even more frequent but unrecognized because declaration of brain death is often a self-fulfilling prophecy: rarely do any life-sustaining interventions continue after the diagnosis is made.
To be consistent, transparent, and accurate, the cessation of function in both the cardiopulmonary and the neurological standard of the UDDA should be described as permanent (i.e., no reversal will be attempted) rather than irreversible (i.e., no reversal is possible). We recognize additional challenges in complying with the UDDA requirements that these cessation criteria for brain death include “all functions” of the “entire brain.” In the absence of universally accepted and easily implemented testing criteria, there may be real problems with being in perfect compliance with these legal criteria in spite of being in perfect compliance with the currently published medical guidelines. If the concept of brain death is philosophically valid, as we think is defensible, then the diagnostic guidelines should be corrected before any attempt is made to correct the UDDA. They must then “say what they mean and mean what they say” to eliminate any possibility of patients with persistent evidence of brain function, including hypothalamic function, being erroneously declared brain dead.
Given these exigencies, any revision of the UDDA should allow for an opt- out clause, which would enable an individual to 1) stipulate that he or she will only accept a determination of death by cardiopulmonary, and not neurologic, criteria, or 2) accept a brain death exam but refuse an apnea test as part of the determination of death by neurologic criteria. While we would not normally countenance requiring consent (or refusal thereof) for the individual steps of a medical procedure or exam, we accept the arguments in favor of it in this controversial circumstance, in part in order to preserve the acceptability of brain death.
Brain death as a concept and a practical diagnosis is under attack from both sides. One side argues that the cases where the diagnosis has clearly been inaccurate prove that the concept of brain death itself cannot be defended and, therefore, should be abandoned in favor of only the cardiopulmonary criteria. The other side says that the dead donor rule coupled with a diagnosis of brain death is too demanding and, therefore, the current standards of brain death should be relaxed or abandoned. We adhere to a middle ground.
We recognize the importance of a determination of brain death in the process of organ donation. However, we also recognize that this represents its sole utility; termination of futile or nonbeneficial life-sustaining interventions does not require a diagnosis of brain death. Taking the organs from such patients in order to transplant them elsewhere does require a declaration of death as a means of honoring the dead donor rule. If the public is to continue to support brain death as a pathway to organ donation, we must make allowance for those who have serious misgivings about the concept of brain death. Refusal of such a determination must be accepted, whether made in advance and incorporated into an advance directive or made by surrogates on behalf of an incapacitated patient.
Exceptional cases of survival on ventilatory support following a careful and complete brain death diagnosis must give us all pause. Either the fundamental concept of brain death is at fault or the criteria being applied for the diagnosis are; we believe the latter issue is the problem. Therefore, if we are to preserve confidence in the reliability of a brain death diagnosis, we must make the diagnostic criteria more reliable. How this can be done is a subject for a subsequent paper and beyond the scope of this essay, but clearly it would at least require evaluations of hypothalamic function. Until this occurs, we must make allowances for those who express doubts about the process. Only following these revisions and modifications will the concept of brain death be reliably supported and the diagnosis accurately made with newfound moral certainty.
Bioethicists of the Pellegrino Center for Clinical Bioethics: G. Kevin Donovan, MD, MA, is professor emeritus of pediatrics and immediate past director of the Pellegrino Center for Clinical Bioethics at Georgetown University Medical Center. Myles Sheehan, SJ, MD, is director of the Pellegrino Center for Clinical Bioethics and a professor of medicine at Georgetown University Medical Center. James Giordano, PhD, MPhil, is a professor in the departments of neurology and biochemistry at Georgetown University Medical Center and chief of the neuroethics studies program at the Pellegrino Center for Clinical Bioethics. Allen H. Roberts II, MD, is a professor of clinical medicine at Georgetown University Medical Center and a core faculty member at the Pellegrino Center for Clinical Bioethics. Siva Subramanian, MD, is a professor in the departments of pediatrics and obstetrics & gynecology, a core faculty member at the Pellegrino Center for Clinical Bioethics, and emeritus chief of neonatal perinatal medicine and a member of the Interreligious Dialogue on Education at the Woodstock Theological Center at Georgetown University and Georgetown University Medical Center. Claudia R. Sotomayor, MD, MBe, is an assistant professor of medicine and chief of the clinical ethics consultation service at the Pellegrino Center for Clinical Bioethics. Sarah Vittone DBe, MSN, RN, is an assistant professor in the School of Nursing at Georgetown University and a clinical ethicist and core faculty member at the Pellegrino Center for Clinical Bioethics.












Organ transplantation is an emotional, personal process for donors and their families while giving hope to potential recipients who may have waited years for an organ, a scarce resource. The method of determining brain death is burdensome for both families and healthcare providers. To promote trust in medicine and the process of organ transplantation, transparent guidelines for determining brain death are crucial. The authors of this essay raise essential points on introducing opt-out clauses to accommodate different cultural and religious beliefs about death when revising the Uniform Determination of Death Act (UDDA) of 1981. Currently, only New Jersey allows for the declaration of death based solely on the cessation of cardiopulmonary functions. Since many providers have uncertainty about the differences in state law, a universal change would make the decision-making process less ambiguous (Lewis et al. 2016). The authors acknowledge that proponents of cardiopulmonary death find the diagnostic criteria for brain death to be inaccurate, whereas proponents of brain death find the diagnostic criteria too rigid. As technology improves, new and more accurate diagnostic tests will gain traction.
While some may contend that changes to the UDDA are too downstream to resolve the scarcity of organs, the transparency resulting after a revision will foster more dialogue between prospective donors and their healthcare providers when drafting advance directives and signing up as organ donors. Thus, upstream effects would make the process more seamless, comprehensive, and understandable as patients and their families decide to donate. Ultimately, the potentially positive upstream effects would promote beneficence in improving the organ supply while minimizing harm, or nonmaleficence, by reducing the burdens of organ donation when families are uncertain about the diagnostic process for their loved one.
In addition to fostering dialogue, revisions to the UDDA should encompass the humanistic aspects of organ donation. For families, organs procured from their loved ones are a difficult and emotional situation to process. Humanism should become a priority to build trust with families and prospective patients registering as organ donors. Emphasizing humanism in medicine, especially while organs are being procured for donation, involves empathy, compassion, and strong dedication to ensuring patient autonomy. Respect for autonomy, another bioethical principle, can be achieved if families can feel comfortable with the declaration of their loved one’s death based on cultural and religious beliefs. Many religions only accept the cardiopulmonary definition of death, and withdrawing life-sustaining care from a patient pronounced brain dead would be against their tenets (Biel & Durrant 2020). Therefore, the UDDA should be revised to include this point on accommodations while emphasizing the transparency of making timely decisions for donations. Justice would also be promoted by respecting these diverse beliefs, allowing for a more equitable process and treatment of patients overall. In essence, allowing this wish to be followed at the end of life will ultimately instill trust in the organ transplant process, encourage more donors and family support, and improve the lives of those on the waiting list.
References
Biel S, Durrant J. Controversies in Brain Death Declaration: Legal and Ethical Implications in the ICU. Curr Treat Options Neurol. 2020;22(4):12. doi:10.1007/s11940-020-0618-6
Lewis A, Adams N, Varelas P, Greer D, Caplan A. Organ support After Death by Neurologic Criteria: Results of a Survey of US Neurologists. Neurology. 2016;87(8):827-834. doi:10.1212/WNL.0000000000003008