Bioethics and Racism
Selected resources from The Hastings Center.
Bioethics Briefings:
Racism threatens health equity by withholding resources people need for proper health based on morally arbitrary features like skin color. Poor health outcomes can result from racism experienced inside and outside of clinical settings. Racism is in opposition to the principles bioethicists often center in their work such as justice, concern for vulnerable populations, and beneficence. Read our briefing to consider: What are the links between racism, health, and health care?
From Hastings Bioethics Forum:
- After the Election, Our Aging Society Will Still Need Care PolicyAfter the election, the care needs of our aging society will continue to be met by families showing up, day after day. Whether or not our public officials decide to imagine otherwise and commit themselves to policy changes that could prove highly popular, bioethics needs to keep its eyes on the caregivers.
- When Bioethics is Like Surfing: Changing Federal PolicyI was honored (and honestly a bit surprised) to play a pivotal role in a recent federal milestone for patients’ rights. On April 1, the Department of Health and Human Services revised its guidelines to require explicit consent from patients for sensitive medical examinations, including…
- Improving Linguistic Justice and Accessibility in Bioethics WorkBioethicists should practice linguistic justice, making our work accessible to people by using relatable language. It’s key to improving health justice.
- To Reduce Maternal Health Disparities, Expand Medicaid Black women are three times as likely to die from preventable pregnancy-related complications as white women in the United States. There are many reasons for this, but one of them is that Black women have lower rates of health insurance. Without insurance, they cannot afford the pre-pregnancy and prenatal care they need to reduce their maternal mortality rate. A fundamental way to address this problem is to expand Medicaid.
- Bioethicists and Health Care Institutions Must Act Against Florida’s Anti-Immigrant LawFlorida’s new anti-immigrant law, SB 1718, has escaped widespread notice, despite the way it will undermine the mission—and core identity–of not-for-profit hospitals as caring institutions that promote the health of the community. Bioethics and health care institutions must take action.
- Medical Interpretation in the U.S. is Inadequate and Harming PatientsOver the past few decades, many major cities in the United States have become more diverse and gained more residents with limited English proficiency. Health care systems have attempted to accommodate these residents, but their medical interpreter services are inadequate and inefficient. The results can be delayed emergency care for children, an increase in medical errors and health care costs, and a decrease in care quality and patient satisfaction.
- Health Equity Without Ethics Perpetuates MarginalizationTo eliminate a quality metric for clinical ethics is at odds with good clinical practice and it reinforces structural inequality.
- Where is Clinical Ethics in the Revised Hospital Accreditation Standards?The Joint Commission, which accredits our nation’s hospitals, eliminated the sole element of performance that governed clinical ethics services. This decision impedes equity and undercuts progress toward fostering ethical practice in health care.
- Advancing Maternal Health Equity with Data Transparency: The Case of TexasTexas has delayed the release of the full report of the most up-to-date data on maternal health, further threatening the health of marginalized women, children, and families.
- Experiencing Racism: Health Care Professionals Speak Out“My emotions and insecurities were at an all-time high, so much so that I was no longer comfortable coming into work. Do my coworkers also joke about my culture, my skin tone? Do my patients and families feel uncomfortable with me being their nurse? These were the questions I frequently asked myself as I anxiously braced myself for my next shift. I could no longer walk the streets, sidewalks, or even the hospital lobby without believing someone was looking at me because of the color of my skin.” ¬ This quote from Cecilia Igwe-Kalu describes her experience as a nurse confronting racism in health care.
- Bioethics in the MarginsBioethics in the Margins is a new podcast that addresses fundamental moral issues facing society that don’t get the attention they deserve.
- Vaccination Discrimination Goes Against Nursing EthicsSome health care providers are prioritizing patients who are fully vaccinated against Covid-19 over those who are unvaccinated. This is unethical.
- Reckoning with Anti-Black Racism in Bioethics: Key TakeawaysThe field of bioethics has a moral responsibility to respond to the continued racial and health inequities confronting Black, Indigenous, and other people of color. Along with several colleagues, we formed an antiracism task force to interrogate that moral responsibility. Here are key takeaways from a recent panel discussion that we organized.
- Should Covid Vaccination Status Be Used to Make Triage Decisions?As the Covid-19 pandemic continues to strain health systems’ capacity to provide adequate care for critically ill patients, should patients’ vaccination status be considered in making triage decisions? This question sparked debate recently after the leak of an internal memo of the North Texas Mass Critical Care Guideline Task Force that proposed using patients’ Covid-19 vaccination status as a factor to assign intensive care beds.
- Bioethics Must Resist Attacks on Critical Race TheoryIt would be easy for bioethicists, to ignore attacks on critical race theory—not in our wheelhouse, too politically charged, and so on. But the attacks on CRT are squarely relevant to our work.
- New Regulation for Organ Procurement Will Improve Equity and Save LivesIn the more than 35 years since federal legislation created organ procurement organizations (OPOs) to recover organs from deceased donors for transplantation, there has been a disparity in their performance, with the best OPOs recovering organs from four times as many donors as the worst…
- After the Anniversary of Covid, Reckoning with Many New NormalsAnniversaries are complicated. In rehabilitation psychology, the anniversary of an accident that caused a brain or spinal cord injury can be a time for profound gratitude and for grief. Now that we have passed the one-year anniversary of the Covid pandemic, each of us continues to deal with the repercussions and wondering what the “new normal” may look like.
- Vaccine Hesitancy Is No Excuse for Systemic RacismFewer vaccines are going to Black people. While it’s easy to fall back on vaccine hesitancy as an excuse, systemic racism is to blame.
- TV Show Depicts Racism in MedicineThe television show The Good Doctor has always focused on issues of diversity and inclusion in medicine from its storylines to its casting. This week’s episode “Irresponsible Salad Bar Practices” asked an important question: Is medical practice inherently racist? The episode opens with a Black…
- Bioethics, Nazi Analogies, and the Coronavirus PandemicThe year 2020 will be remembered as the first year of the coronavirus pandemic. But the pandemic was not alone in creating fear and dismay and raising ethical questions. Think of the rise in antisemitism, police violence against Black people, protests against immigration, and rallies by groups espousing Nazi slogans and symbols. Hate crimes, including murder, are the highest in years, according to the most recent FBI report, and were particularly aimed at Jews and Hispanics. Asian-Americans have been targeted as carriers of the so-called “China virus.”
- Detention, Dignity, and a Call for Bioethics Advocacy
- Amid the Pandemic and Racial Injustice, Greater Empathy in Medical SchoolEmpathy does not need to dissipate as we endure medical training. Both the pandemic and the national reckoning over racial injustice and police brutality have touched every aspect of life as we know it, and medical training and education have been no exception.
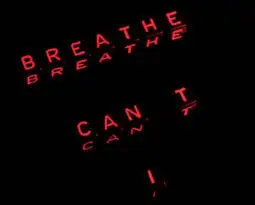
- Black Women Can’t BreatheYears before George Floyd begged to be released from under the knee of Officer Derek Chauvin, Barbara Dawson, a 57-year-old Black woman, died begging a police officer, John Tadlock, not to remove her oxygen mask. Her death occurred right outside the Calhoun Liberty Hospital in Blountstown, Florida, shortly before Christmas in 2015.
- Are Physicians Hypocrites for Supporting Black Lives Matter Protests and Opposing Anti-Lockdown Protests? An Ethical AnalysisPhysicians have been vocal in condemning the anti-lockdown protests while endorsing and even participating in the Black Lives Matter protests. This has led to criticism of the medical community for being inconsistent and hypocritical. What does an ethical analysis reveal?
- Hacking Ventilators in a PandemicThe Covid-19 pandemic continues to test and occasionally overwhelm health care institutions. Many practitioners may face the ethically challenging scenario of having to ration ventilators while triaging patients in “crisis care.” Ventilator shortages have led to innovative ventilator design “hacks.” Are these improvised ventilators ethical?
- Black Bioethics and How the Failures of the Profession Paved the Way for Its ExistenceIn many ways, black bioethics can be explained very simply as the exploration and interrogation of any event, ideal, technological advancement, person, or institution that directly or indirectly affects the health or well-being of black (loosely defined) individuals or the black population. Black bioethics is taking what we do in bioethics and specifically applying it to black people. But in other ways black bioethics is more than this; it is a rebellion against bioethics.
- Ethicists as a Force for Institutional Change and Policies to Promote EqualityIn his recent JAMA article, Donald Berwick eloquently describes what he termed the “moral determinants of health,” by which he meant a strong sense of social solidarity in which people in the United States would “depend on each other for securing the basic circumstances of healthy lives,” reflecting a “moral law within.” Berwick’s work should serve as a call to action for bioethicists and clinical ethicists to consider what they can do to be forces of broad moral change in their institutions.
- Cracks in the System: Lessons Learned from the Covid-19 PandemicThe United States leads the world in coronavirus cases and deaths. Although many people have called out the inadequacies of our health care system, Covid-19 has exposed the most significant shortcomings. The need for change can no longer be ignored. Here are three lessons from this pandemic that should be leveraged for change.
- Committing to Fight RacismWe have reached a very sad, painful moment in the United States. It feels like a cascade of calamities, one compounding the next. An infectious disease pandemic that we cannot yet cure has precipitated an economic crisis. An episode of police brutality against a black man has added the name George Floyd to a long list of victims of unfair policing practices in black communities. Bioethicists have not been doing enough in our professional capacities to actively denounce or address the persistent problems of structural racism. We invite our fellow bioethics colleagues to join us in candid, uncomfortable conversations about what we can and should be doing differently.
- Immigrant Health and the Moral Scandal of the “Public Charge” RuleA long-anticipated policy change proposed by the Trump administration that would count the use of many federally-subsidized programs against immigrants currently eligible to use them threatens public health and would undermine ethical practice in health professions and systems. The policy would expand the definition of…
- A Single-Payer Bubble?In an earlier piece, “Trumping Drug Costs,” I looked at out-of-pocket costs as the pivotal issue with drugs. They can be a particularly heavy burden on the elderly, taking money from their savings and a large bite of their Social Security income. Along the way,…
- Trumping Drug CostsI usually have trouble finding a good word to say for President Trump’s policy ventures, but his aim to better control out-of-pocket drug costs is worth support. Distressingly, but unsurprisingly, it does not include giving government the needed power to bargain with industry for what…
- Is it Time to Regulate the Sale of Sugar to Minors?In “Tackling Obesity and Disease: The Culprit Is Sugar; the Response is Legal Regulation,” published in the Hastings Center Report, Lawrence O. Gostin describes four coordinated interventions that have been effective at controlling peoples’ tobacco consumption and which can serve as a “powerful model” for…
- Organ Donation and Transplantation in the U.S.: 50 Years of Success, Strategies for ImprovementThe Uniform Anatomical Gift Act, a landmark law adopted 50 years ago this summer, has provided a sound and stable legal platform on which to base an effective nationwide organ donation and transplantation system, as we discuss in our article in the current issue of…
- When Pat and Bob Nearly Saved Health Care Reform: A Lesson in Senatorial Bedside MannerWith Senator John McCain’s heroic return and Vice President Mike Pence’s tie-breaking vote on a health care bill July 25, Senate Republicans managed to cobble together 51 votes simply to agree to debate health care reform. This razor’s edge victory is diagnostic. Hyperpartisan debate is convulsive. It endangers…
- Morally Indefensible Health Care BillsThere is a broad and deep moral conviction that health care should be distributed according to genuine need and not left to the cold mercy of pure market forces or the logic of actuarial fairness. Unfortunately, the proposed American Health Care Act (AHCA), passed last week in the House of Representatives, and other legislation threaten to undermine that moral commitment.
- Health Reform and Competing Visions of JusticeOn May 4, 2017, just over one month after abandoning a previous version of the bill, the U.S. House of Representatives voted by a 217-213 margin (with one abstention) to adopt the American Health Care Act (AHCA). During the coming weeks and months, most of…
- How “America First” Undermines Our HealthPeople value their health. It allows them to pursue their aims and enjoy their lives, and it contributes to their well-being. But health is not only good for particular healthy individuals. It is also good for their families, communities, nations, and in a world in…
- After the Election Bioethics Faces a Rocky RoadAcademic bioethics has never been popular with Republicans. Libertarians dislike academic bioethics because it seems too elitist and anti-free market. Religious thinkers worry it is technocratic, soulless and crassly utilitarian. Now with Trumpism add a populist disdain for expertise, experts and the scientific method and…
- The Challenge of High Drug Prices in the U.S.Drug spending in the United States increased more than 12 percent in 2014 and is projected to rise faster than overall health care spending over the next 10 years. Between 2007 and 2016, the price of a pair of epinephrine autoinjector EpiPens, used to counter…
- The Good of the BodyThe December 2015 United Nations meeting on climate change was an historic moment for global efforts to reduce harmful carbon emissions. While it gained the agreement about the future good of the planet, it made clear that there is a long and hard road still…
- Right to Try Laws and the Power of StoriesI said that in focusing on abstract science and policy arguments against right to try laws, experts (and here I meant to include ethics experts) have neglected the power of stories. Patients’ stories are the currency of right to try advocates. But the stories advocates…
- The Supreme Court and Health Care Access for Undocumented ImmigrantsThe Supreme Court announced that it will hear a legal challenge to President Obama’s 2014 executive action to protect an estimated five million undocumented immigrants from deportation and permit them to work legally. The implementation of the Deferred Action for Parents of Americans and Lawful Permanent Residents…
- After Banning Torture, Psychology Association at a CrossroadsThe American Psychological Association (APA) voted at its 2015 meeting to ban psychologists from participating in national security interrogation programs, including torture. The policy change was in response to the public outcry over the release of unsettling Senate Intelligence Committee’s report on the Central Intelligence Agency’s detention and interrogation…
- Reasonable Regulation of Surrogate MotherhoodThis month France’s highest court granted legal recognition to children born to surrogates. Previously, surrogate children were deprived of any legal connection to their parents, or any civil status in France. They could not get ID cards or passports, or register for state health care…
- California’s Strides in Providing Health Care for Undocumented ImmigrantsI had just turned 5 in November 1994 when my fellow Californians voted to pass Proposition 187 in a draconian attempt to restrict undocumented immigrants from receiving health care, education, and other services, as well as to require doctors, teachers, and others to report those suspected of…
- Supreme Court Decision in King v Burwell: Backstory and Next StepsThe Patient Protection and Affordable Care Act (ACA) relies on three primary strategies for expanding health insurance coverage. First, it regulates the insurance market to prevent practices that made it difficult or impossible for sick people to purchase insurance. Second, it expands Medicaid dramatically, particularly for childless…
- When Words Matter: Medical Education and the Care of Transgender PatientsI was only there to learn how to place IV lines. But as my anesthesia attending and I gathered our needles, tourniquet, and gauze, I noticed that our patient, whom I’ll call Jamie, didn’t appear to fit into a narrowly defined version of gender. I…
- Don’t Categorically Refuse CPR to Ebola PatientsRecently it has been argued that cardiopulmonary resuscitation (CPR) should, as a matter of policy, not be offered to persons with Ebola disease. Such a categorical restriction of CPR based solely on a patient’s diagnosis rather than his prognosis would be unique in modern medical…
- Responding to Ebola: Questions about ResuscitationWhile details of the deaths of patients in Dallas and Madrid from Ebola are not public, their passing prompts questions about resuscitation in individuals infected with the virus. To date, this question has not been raised in clinical ethics. We must now consider whether unilateral…
- New York City’s Innovative Approach to Helping Unaccompanied MinorsNew York City Mayor Bill de Blasio recently announced a plan to connect unaccompanied minors who have arrived in the city from Central America with public education and health care through the legal system. Between January 31, 2014 and August 31, 2014, 4,799 children have been released to sponsors…
- Responding to Ebola: Retrofitting Governance SystemsIn a recent New York Times op-ed, David Brooks observes that governance, in the form of multilateral organizing, is missing from the response to the Ebola epidemic in West Africa. Unfortunately, global organization and health infrastructure building too often occur in the midst of a public health emergency. A…
- Responding to Ebola: Organizational Ethics, Frontline PerspectivesBeyond crucial questions of fair access to scarce supplies of the experimental drug ZMapp and to other potentially effective drugs to treat Ebola, commentators from bioethics, public health, journalism, and other sectors are increasingly focused on “staff, stuff, and systems.” The consequences of chronically inadequate local and…
- FDA Proposal for Regulating Laboratory Diagnostics Could Improve Patient CareWendy Chung’s commentary last month about the FDA’s proposed draft guidance for the regulation of laboratory-developed tests (LDTs) is heavily critical of the agency’s plans. Professor Chung argues that the FDA’s involvement in this space will have two primary negative consequences: it will stifle innovation and it…
- The VA Crisis is Fundamentally an Ethics CrisisThe crisis and failure of caregiving that have engulfed the Veterans Health Administration cannot be solved with increased resources or even by hiring more doctors and nurses. Additional resources are critical and necessary—but they are not a sufficient long-term and comprehensive solution to a problem…
- Hobby Lobby Decision Likely to Increase Health Care InequityThe Supreme Court’s ruling in Burwell, Secretary of Health and Human Services, et al. v. Hobby Lobby Stores, Inc., et al., could undermine a central goal of the Patient Protection and Affordable Care Act (ACA): to expand access to health care by creating a system in…
- What Do We Owe to Child Migrants?From October 1, 2013, through June 15, 2014, more than 52,000 child migrants crossed the U.S.-Mexico border in South Texas, overwhelming the U.S. Customs and Border Patrol and the Department of Homeland Security (DHS). The Obama administration has declared this an “urgent humanitarian situation” and has authorized…
- Despite the Risks, and Because of Them, the FDA Should Permit Recycling Medical ImplantsIt is hard to quibble with the fact that Dr. Daniel Mascarenhas is breaking the law. It is also hard to quibble with the fact that he is a hero. The doctor is breaking the law as he tries to find pacemakers from those who have…
- What Role Should Bioethics Play in Global Health?I appreciate Dr. Benatar’s essay on the role of bioethics in confronting the challenges of global health inequities. His article aptly catalogues the contributing factors–both specific to health and otherwise–that weigh heavily on our unequal world. More importantly, Dr. Benatar’s focus on the role that bioethics ought…
- How Bioethicists Can Help Reduce Global Health InequitiesThe state of global health is a major concern. Despite advances in medicine and medical care and massive growth of the global economy, health in the world is characterized by widening disparities within and between countries; lack of access to even basic health care for…
- Truvada: No Substitute for Responsible SexA new debate is surging through the gay male population in the United States: should gay men take a drug that can reduce their risk of contracting HIV? The drug in question is Truvada, a combination antiretroviral commonly used to treat HIV infection. In 2012,…
- “Health Care as Hospitality”: Organizational Ethics in a Migrant Health ClinicGeylang is the red-light district of Singapore, east of the city center. It would be easy, and wrong, to describe Geylang as a different world from the skyscrapers and malls of the contemporary, booming city. Its restaurants and its vernacular “shophouse” architecture link its street…
- Bloomberg, Nannying, and the Symbolic Value of Food ChoiceI mostly agree with Lawrence Gostin’s paean to outgoing New York City Mayor Michael Bloomberg in the Hastings Center Report. Like Gostin, I see Bloomberg as a public health innovator who has tested the boundaries of government power in productive ways. Gostin helpfully summarizes—and then…
- Bloomberg’s Health Legacy: What Inflames Consumer Passions in the Food Wars?After the Hastings Center Report published my essay on Mayor Bloomberg’s health legacy — with its key ideas spread through the popular media (here and here) — vitriolic messages streamed into my inbox. The messages were not intellectual arguments supporting free enterprise or limited government….
- Why Health Plan Cancellations Do Not Mean Failure for ACAOn November 14, President Obama announced that he would delay by one year the implementation of requirements imposed by the Patient Protection and Affordable Care Act(ACA) that would have led to the cancellation of some low cost health insurance plans. The president felt compelled to…
- In Search of SterilityIn the November-December issue of the Hastings Center Report I wrote about voluntary sterilization for childfree women. The article came about through my inability to get sterilized as a childfree woman. I had never wanted children. In college I met a man who felt the same way….
- “Poverty Impedes Cognitive Function” – Reason to Help, or Blame, the Poor?“’The lower the caste,’ said Mr. Foster, ‘the shorter the oxygen.’ The first organ affected was the brain. After that the skeleton.” In Brave New World cognitive ability is carefully and intentionally bred out of the lowest rungs of society. Although he was writing fiction, Aldous Huxley…
- Charging Smokers Higher Health Insurance Rates: Is it Ethical?Smoking-related illnesses cost the United States hundreds of billions of dollars a year in health care expenditures and lost productivity, and claim hundreds of thousands of lives.” Given the enormous medical and economic toll of smoking, it is not surprising that 58 percent of Americans favor charging…
- The Supreme Court and the Fight Against AIDSThe salience of the Constitution’s spending clause to the public’s health is not often appreciated–empowering the federal government to “provide for the common Defense and general Welfare.” But the power to spend–along with the equally vital power to tax–provides government with authority to allocate vast…
- “Undocumented Doctors” and the Health of the DreamersLoyola University Chicago Stritch School of Medicine’s recent announcement that it would accept applications from Dreamers – young undocumented immigrants eligible for Deferred Action on Childhood Arrivals (DACA)status – is an innovative and welcome response to the promise implicit in DACA. The idea that young people who had been…
- Sports Concussions and SandbaggingSport-related concussions are a significant public health problem, and concussion management is one of the most controversial issues in sports medicine. The latest international consensus statement on concussion in sport advises that players not return to play on the same day they were injured and that they…
- Touching HistoryAIDS in New York: The First Five Years is an exhibit running this summer at The New-York Historical Society, an organization so venerable that its name reflects how the city’s name was originally spelled. The exhibit works on several levels: historically, as a story about how…
- Learning to Talk Like a DoctorThree years before beginning medical school, I got off a bus in Granada, Spain and met the family I would be living with for four months. My host parents, Carmen and Monolo, introduced themselves and asked how old I was, where I was from, and…
- Why Target National Obesity Rates?In a recent article in the Hastings Center Report, Daniel Callahan argues that obesity is a serious public health problem facing the U.S. and suggests a variety of strategies for combating this problem. The article has provoked a great deal of public attention on blogs and web news…
- Why Target National Obesity Rates?In a recent article in the Hastings Center Report, Daniel Callahan argues that obesity is a serious public health problem facing the U.S. and suggests a variety of strategies for combating this problem. The article has provoked a great deal of public attention on blogs and web news…
- A More Ethical Strategy Against Obesity: Changing the Built EnvironmentSince the 1960s, obesity has become one of the most significant health problems in industrialized nations. In the U.S., the percentage of obese adults increased from 13 percent in the 1960s to 32 percent in 2004. According to some estimates, 41 percent of U.S. adults will be obese…
- Obesity and Public Health: No Place for ShameIn his article, “Obesity: Chasing an Elusive Epidemic,” published in the Hastings Center Report, Daniel Callahan posits that obesity is so widespread and embedded in our culture that most if not all efforts to combat it have failed, and failed miserably. Change, in a large and…
- Controversy in the Hastings Center Report: Responding to an Article on ObesityNearly everyone agrees that obesity is a significant public health problem in the United States, and nearly everyone agrees that the public health responses to it so far have been disappointing. So what should be done about it? In the January-February issue of the Hastings Center Report,…
- Rites and Wrongs: Changing a Ritual from WithinThe previously obscure ultra-Orthodox Jewish rite of metzitzah b’peh (oral suction) has burst into the news lately and raised critical questions about genital surgery, consent, First Amendment rights, tradition, and the representation of Jews. I would guess that most Americans, even Jewish-Americans, had never heard…
- What Can Plato Teach Us About the Health Insurance Mandate?As any philosopher worth his or her salt can tell you, health insurance is not among the array of topics in Plato’s corpus. Even so, a lesson on citizenship from one of his more famous dialogues, “Crito,” can teach why the insurance mandate in the…
- The Hazards of Fast ScienceA recent editorial in Nature lauds the U.S. government for its efforts to promote open communication between government scientists and journalists, but it condemns the Canadian government for its opposing efforts to limit what federal scientists can freely communicate to journalists. TheNaturecriticisms of the Harper government are…
- Pink Ribbons, Wire Hangers, and the Politics of Women’s Health“Pink is the new wire hanger.” In the flurry of tweets that followed in the wake of the debacle between Susan G. Komen for the Cure and Planned Parenthood, this one was my favorite. It combined two powerful symbols in women’s health–the pink ribbon of the breast…
- Medicine as a Weapon in Syria and BeyondA recent editorial in The Lancet issued a dire warning to the international medical community: medicine is a weapon of war in Syria. It is just the latest in a series of reportsfrom across the Middle East on how medical care and medical professionals and facilities are…
- Justified Restrictions on Religious FreedomThe Obama administration’s decision regarding Catholic institutions and coverage for reproductive health has stirred up a firestorm of claims that the policy restricts religious freedom. That’s true: the policy does restrict religious freedom to an extent. But while freedom of religion is surely a principle Americans…
- A Lesson from the Contraception Coverage Uproar? Rethink Employer-Based InsuranceUnless you’ve been living under a rock for the past few weeks, you’re now well aware of the otherhealth care mandate. The Affordable Care Act requires insurers to cover “preventative health services” without charging a copayment, co-insurance, or a deductible, and the Obama administration has interpreted this requirement…
- Health Workers as Pawns of WarfareLast week, NPR reported a major humanitarian group’s decision to stop treating patients from detention centers in Misrata, Libya. According tothe report,“torture was so rampant that some detainees were brought for care only to make them fit for further interrogation.” While it must have been…
- Obama’s Unspoken Words About Health Reform and ValuesMany in the health policy world worried when President Obama made only passing reference to health care in his State of the Union Address — only two mentions of the words “health care” and one each for “Medicaid” and “Medicare.” While there may be a…
- It’s Not Just the Economy, StupidDespite the persistent focus on economic growth, jobs, and global competition in the Republican presidential primaries, many social issues with significant bioethics implications are also at stake in November’s election. Given the importance of science and health policy, it is worth exploring the positions of…
- The American Medical Association’s Apology in Context: The Need for RestorationThe AMA’s recent apology to black physicians marks another moral milestone in white America’s ritualized confession of its racist past, standing alongside President Clinton’s 1997 apology to the survivors of the American government’s infamous syphilis study of black males. The AMA’s commissioned research panel previously…
- When HIPAA HurtsEver since HIPAA went into effect and I’ve been signing that form over and over at my doctors’ offices, attesting to my knowledge of the law, I’ve been feeling I should turn the tables and make my doctors and their staffs sign some form assuring…
- The Federal Marriage Amendment and the New One Drop of Blood RuleAs anti-miscegenation laws took hold in an effort to stop blacks and whites from marrying, by necessity courts had to start deciding who counted as white or black. The standard that ultimately emerged – namely the “one drop of blood” rule of blackness – dictated…
From Hastings Center Report:
To Understand Inequity, Bioethics Needs to Sort Things Out
First published: 24 April 2023
Abstract
Bioethics is reexamining how to implement diversity, equity, inclusion, and justice concerns into scholarship. However, bioethicists should question the categories used to define diversity. The act of categorization is value laden, and classification systems confer power and benefits and generate harms. For example, what conditions count as disabilities? We should consider the equity implications of offering only “male” and “female” options for self-identification in health records. However, we should also interrogate all ideas about categorization, including how categories are formed, why they are formed, and who decides. Bioethicists cannot comprehend fully what equity and justice mean for underrepresented, underserved, or marginalized people until there is an understanding of how the boundaries of marginalization are created.
An Ecostructural Lens for Health Ethics
First published: 20 December 2022
Abstract
In this commentary, I describe an ecostructural approach to health ethics, which is grounded in a conception of people as ecological subjects and privileges place in supporting health and health justice. This approach sees people as dwelling in health ecosystems that can support or undermine health, and it situates us in social norms and processes, with a particular concern for structural health injustice. In patient care, an ecostructural approach can be operationalized by attending to conditions in the sites where birthing, healing, and dying take place and by critiquing their economic structures. For public health, relationships between people, animals, land, the built environment, and climate demand attention, as do racist norms and economic processes that thwart health justice. For global health, an ecostructural approach might envision a revolution in governance that challenges nationalism, in which health systems treat citizens while depending on human resources supplied through structures that sustain health injustice.
Do Health Care Organizations Have Legitimate Responsibilities beyond the Delivery of Health Care? Insights from Citizenship Theory
First published: 22 August 2022
Abstract
Many health care organizations made public commitments to become antiracist in the wake of George Floyd’s murder. These actions raise questions about the appropriateness of health care’s engagement in racial justice and social justice movements generally. We argue that health care organizations can be usefully thought of as having two roles: a functional role to care for the sick and a meta-role as an organizational citizen. Fulfilling the role of citizen may require participating in the pursuit of social justice, including efforts to achieve racial equity. The demands of these two roles will need to be balanced, but the role of organizational citizen has been largely ignored and merits serious attention.
DEI Is Not Enough
First published: 28 June 2022
Abstract
The movement under way to increase diversity, equity, and inclusion (DEI) in every workplace, including academia, medicine, and science, is an essential step toward health justice, but only a first step. Bioethics, health care, and health-related research all need more professionals from minoritized groups, but all of us need to do more to address justice at every level. From inclusive workplace policies and practices to research into structural injustices and health disparities, bioethics can and must lead the way in collaborative efforts. The work belongs to all of us, and DEI is only the beginning.
New Findings on Unconsented Intimate Exams Suggest Racial Bias and Gender Parity
First published: 27 April 2022
Abstract
Testimony from hundreds of medical students and numerous physicians and scholars suggests that unconsented intimate exams (UIEs) are unlikely to be rare, isolated incidents. However, much is unknown about the frequency of these exams and the circumstances in which they take place. The Community Bioethics Forum, founded and chaired by one of the authors of this commentary, is a consultative group of diverse community members who provide insights on law and policy to policy-makers and medical associations. Connecticut legislators asked the CBF to provide their views on proposed “explicit consent” legislation, and during those discussions, concerning narratives emerged about members’ (and their loved ones’) personal experiences with UIEs.
To gain greater clarity on the demographic patterns and frequency of UIEs, we conducted the first national survey on UIEs. Data from this survey suggest that UIEs may occur under a broader range of circumstances than addressed by most law and policy. The survey resulted in nearly the exact same rate of affirmative responses between males and females in answer to whether they had received a UIE within the past five years. The survey results also showed evidence of racial disparity. Additional research is needed to understand the nature of UIEs.
Structural Inequities, Fair Opportunity, and the Allocation of Scarce ICU Resources
First published: September 2021
Abstract
The September-October 2021 issue of the Hastings Center Report highlights the important topic of allocating scarce critical care resources during the Covid-19 pandemic. The article by Alex Rajczi and colleagues urges that policy-makers use public reasoning, not private reasoning, when developing triage policies. We completely agree. We show how the allocation framework we developed as private scholars, the “Pittsburgh framework,” has been supported by public reasoning.
The article by Mary Katherine Gaurke and colleagues criticizes rationing based on maximizing life-years saved and mistakenly claims that our framework recommended this approach. We explain that our framework never contained such a criterion but instead included a more limited consideration of near-term prognosis. In December 2020, in response to emerging data and important criticisms, we modified our framework to further strengthen equity. We are committed to improving allocation guidelines during crisis standards of care through reflective discussions and debates.
Against Exclusive Survivalism: Preventing Lost Life and Protecting the Disadvantaged in Resource Allocation
First published: 16 September 2021
Abstract
When life-saving medical resources are scarce and not everyone can be saved, is the only relevant goal saving the most lives? Or can other factors be considered, at least as tiebreakers, such as how early in life the people we don’t save will die or how much future life they are likely to lose? This commentary defends a multiprinciple allocation approach that considers objectives in addition to saving more lives, including preventing early death and preventing harm in the form of lost future life. Particularly compared to an arbitrary, coin-flip tiebreaker, this multiprinciple approach more effectively prevents harm, prioritizes the worst-off, mitigates socioeconomic and racial health disparities, and tracks public values regarding allocation under scarcity—and is legally sound.
Crisis Standards of Care—More Than Just a Thought Experiment?
First published: 16 September 2021
Abstract
As described in two articles in the September-October 2021 issue of the Hastings Center Report, most crisis standards of care (CSC) plans include triage algorithms to guide the allocation of critical care resources to some patients and not others under conditions of extreme scarcity. The plans also include other important CSC strategies, but it is the notion of rationing scarce resources via triage that especially captured the imaginations of ethicists. Vigorous arguments have arisen over whether triage algorithms should be designed to prioritize patients based on predictions of short-, near-, or long-term survival. Additionally, there are ongoing debates about the ability of current algorithms to estimate patient survival accurately enough to be useful in triage and about the role of values like equity in triage protocols. Relatively few debates have noted, however, that while the development of CSC triage protocols has been based in medicine, public health, and ethics, the activation of CSC plans remains a political decision.
Antiracist Activism in Clinical Ethics: What’s Stopping Us?
First published: 13 July 2021
Abstract
Although justice is a central principle in clinical ethics, work that centers social justice is often marginalized in clinical ethics. In addition to institutional barriers that may be preventing clinical ethicists from becoming the activists that Meyers argues we should be, we must also recognize the barriers embedded in the field of clinical ethics itself. As clinical ethicists, we have an opportunity to support anti-racism work in particular by altering our own organizational structures to be more inclusive and reflective of the Black, Indigenous, and other communities of color we serve, enhancing clinical ethics education and training by making critical theories foundational, and decolonizing our clinical ethics consultation tools and practices.
History and Bioethics
First published: 11 April 2021
Abstract
Cultural historians and historians of medicine are a rarity in bioethics. Even those who write histories of bioethics are philosophers, sociologists, or theologians. Where have all the historians gone? If bioethics is to contribute to the urgent work of addressing social justice, structural racism, and health inequity, we bioethicists need to embrace history as a fully constituent part of our field. Historians can help us apprehend the ideas that shaped bioethics, and health policy more broadly, and discover the dissenting arguments that might inspire us now. Given our annus horribilis, history has become an instrumental necessity. It is only through the study of history that we can understand the past so as to reimagine how bioethics can influence health policy and work toward health equity.
Antiracist Praxis in Public Health: A Call for Ethical Reflections
First published: 11 April 2021
Abstract
The Covid-19 pandemic has revealed myriad social, economic, and health inequities that disproportionately burden populations that have been made medically or socially vulnerable. Inspired by state and local governments that declared racism a public health crisis or emergency, the Anti-Racism in Public Health Act of 2020 reflects a shifting paradigm in which racism is considered a social determinant of health. Indeed, health inequities fundamentally rooted in structural racism have been exacerbated by the Covid-19 pandemic, which calls for the integration of antiracist praxis to promote ethical public health research processes. This commentary describes ways in which antiracist praxis—which emphasizes empowerment of traditionally marginalized populations—offers strategies to explicitly address power imbalance, stigmatization, and other consequences of structural racism in public health research.
Residential Segregation and Publicly Spirited Democracy
First published: 25 February 2021
Abstract
Successful deliberations over contentious issues require a publicly spirited citizenry that will encourage elected officials to promote what James Madison called the “permanent and aggregate interests” of the country. Unfortunately, atomizing forces have pulled American society apart, undermining trust and making collective action difficult. Residential segregation is one of those atomizing forces. Residential segregation undermines a commitment to civic virtue because it encourages people to think about fellow citizens as “others” with whom they have little in common. To address this situation, we must start by fixing our neighborhoods and creating local institutions that enhance trust and foster a public-spirited democratic citizenry. For example, our existing educational policies reinforce the disparities associated with residential segregation and have created massive resource inequalities among school districts across the country. A useful first step would be to equalize school district funding to promote a more genuine equality of opportunity.
Civic Learning, Science, and Structural Racism
First published: 25 February 2021
Abstract
Vaccine hesitancy is a major public health challenge, and racial disparities in the acceptance of vaccines is a particular concern. In this essay, we draw on interviews with mothers of Black male adolescents to offer insights into the reasons for the low rate of vaccination against the human papillomavirus among this group of adolescents. Based on these conversations, we argue that increasing the acceptance of HPV and other vaccines cannot be accomplished merely by providing people with more facts. Instead, we must address the pervasive racial discrimination in the United States that undermines trust in social institutions, including the health care system. In the short term, it may be helpful to increase the number of clinicians of color working in the health system, but more fundamental changes are required. The U.S. must adopt and implement policies that dismantle structural racism if it hopes to produce greater trust and community-oriented thinking on behalf of people who have been exploited for centuries.
The Emerging Hazard of AI-Related Health Care Discrimination
First published: 14 December 2020
Abstract
Artificial intelligence holds great promise for improved health-care outcomes. But it also poses substantial new hazards, including algorithmic discrimination. For example, an algorithm used to identify candidates for beneficial “high risk care management” programs routinely failed to select racial minorities. Furthermore, some algorithms deliberately adjust for race in ways that divert resources away from minority patients. To illustrate, algorithms have underestimated African Americans’ risks of kidney stones and death from heart failure.
Algorithmic discrimination can violate Title VI of the Civil Rights Act and Section 1557 of the Affordable Care Act when it unjustifiably disadvantages underserved populations. This article urges that both legal and technical tools be deployed to promote AI fairness. Plaintiffs should be able to assert disparate impact claims in health-care litigation, and Congress should enact an Algorithmic Accountability Act. In addition, fairness should be a key element in designing, implementing, validating, and employing AI.
Between Crisis and Convention: How Should We Address Contingency?
First published: 23 October 2020
Abstract
The Covid-19 pandemic has brought about renewed conversation about equality and equity in the distribution of medical resources. Much of the recent conversation has focused on creating and implementing policies in times of crisis when resources are exhausted. Depending on how the pandemic develops, some communities may implement crisis measures, but many health care facilities are currently experiencing shortages of staff and materials even if the facilities have not implemented crisis standards. There is a need for shared conversation about equality and equity in these times of contingency between conventional and crisis medicine. To respond well to these challenges, I recommend that institutions rely on policy, professional education, and ethics consultation. As is the case with crisis policies, creating contingency policies requires that health care professionals decide on how, specifically, to achieve equity. A policy is only as effective as its implementation; therefore, institutions should invest in context-specific education on contingency policies. Finally, ethics consultation should be available for questions that contingency policies cannot address.
The Future of Bioethics: It Shouldn’t Take a Pandemic
First published: 29 June 2020
Abstract
The Covid-19 pandemic has concentrated bioethics attention on the “lifeboat ethics” of rationing and fair allocation of scarce medical resources, such as testing, intensive care unit beds, and ventilators. This focus drives ethics resources away from persistent and systemic problems—in particular, the structural injustices that give rise to health disparities affecting disadvantaged communities of color. Bioethics, long allied with academic medicine and highly attentive to individual decision-making, has largely neglected its responsibility to address these difficult “upstream” issues. It is time to broaden our teaching, research, and practice to match the breadth of the field in order to help address these significant societal inequities and unmet health needs.
Black Lives in a Pandemic: Implications of Systemic Injustice for End-of-Life Care
First published: 29 June 2020
Abstract
In recent months, Covid-19 has devastated African American communities across the nation, and a Minneapolis police officer murdered George Floyd. The agents of death may be novel, but the phenomena of long-standing epidemics of premature black death and of police violence are not. This essay argues that racial health and health care disparities, rooted as they are in systemic injustice, ought to carry far more weight in clinical ethics than they generally do. In particular, this essay examines palliative and end-of-life care for African Americans, highlighting the ways in which American medicine, like American society, has breached trust. In the experience of many African American patients struggling against terminal illness, health care providers have denied them a say in their own medical decision-making. In the midst of the Covid-19 pandemic, African Americans have once again been denied a say with regard to the rationing of scarce medical resources such as ventilators, in that dominant and ostensibly race-neutral algorithms sacrifice black lives. Is there such thing as a “good” or “dignified” death when African Americans are dying not merely of Covid-19 but of structural racism?
Experiencing Community in a Covid Surge
First published: 05 May 2020
Abstract
As I organize a pile of ethics consult chart notes in New York City in mid-April 2020, I look at the ten cases that I have co-consulted on recently. Nine of the patients were found to be Covid positive. The reasons for the consults are mostly familiar—surrogate decision-making, informed refusal of treatment, goals of care, defining futility. But the context is unfamiliar and unsettling. Bioethicists are in pandemic mode, dusting off and revising triage plans. Patients and potential patients are fearful—of the disease itself and of the amplification of health disparities and inequities. There is much to contemplate, but as I go through my cases, I worry about disability, about biases and racist stereotypes. In this pandemic, historically marginalized communities are at risk of further disenfranchisement.
Trust, Risk, and Race in American Medicine
First published: 18 February 2020
Abstract
There is ample evidence that patient mistrust toward the American medical system is to some extent associated with communal and individual experiences of racism. For groups who have faced exploitation and discrimination at the hands of physicians, the medical profession, and medical institutions, trust is a tall order and, in many cases, would be naive. Nevertheless, trust is often regarded as a central feature of the physician-patient relationship. In this article, I draw on empirical research, ethical theory, and clinical cases to propose one way that providers might address and, ideally, resolve mistrust when it arises in an immediate case.
I describe how medical mistrust has been characterized empirically within medical and bioethics scholarship, and I provide an overview of theories of trust, arguing that they may be unable to account for the risks that providers must take in seeking to establish trust within many American medical institutions. Common assumptions in medical and bioethical scholarship on trust notwithstanding, caring and competence are not always enough to establish a trusting relationship between physician and patient. I suggest that, in an atmosphere of mistrust, comprehension of the existence and source of suspicion is essential to effective signaling of trustworthiness.
Earning Patient Trust: More Than a Question of Signaling
First published: 18 February 2020
Abstract
Laura Specker Sullivan’s article “Trust, Risk, and Race in American Medicine” is a philosophically grounded and highly practical call for medical professionals to take on the task of comprehending the sources of patients’ mistrust. This is not only a clinical competence but also a moral obligation, in particular, when mistrust is warranted—as with African American patients who rely on medical institutions that have breached and continue to breach the trust of their communities. While Specker Sullivan focuses on how clinicians can signal comprehension once it has already been attained, I wish to step back and examine the nature of the efforts to gain knowledge. The effort to comprehend requires, at a minimum, the following actions: educating oneself about medical racism, examining one’s implicit biases, and engaging, with empathic curiosity, with the patient or family members in the clinical encounter at hand.
Laypeople Are Strategic Essentialists, Not Genetic Essentialists
First published: 03 July 2019
Abstract
In the last third of the twentieth century, humanists and social scientists argued that attention to genetics would heighten already-existing genetic determinism, which in turn would intensify negative social outcomes, especially sexism, racism, ableism, and harshness to criminals. They assumed that laypeople are at risk of becoming genetic essentialists. I will call this the “laypeople are genetic essentialists model.” This model has not accurately predicted psychosocial impacts of findings from genetics research. I will be arguing that the failure of the model can be traced to its inability to recognize the complexity of laypeople’s attitudes; its incorrect theory of how beliefs, attitudes, and discourse function; and its blindness to how academics’ own interests can override the available evidence. More specifically, I suggest that the substantial data about laypeople’s deployment of genetics supports what I will call the “laypeople are strategic essentialists model” better than the “laypeople are genetic essentialists model.” The strategic essentialists model holds that people tend to store multiple categories, including multiple causal forces, that they deploy “strategically” to serve context-dependent goals. It will be difficult for academics to reorient ourselves to model laypeople as sophisticated strategic essentialists rather than as naïve genetic essentialists. Perhaps a little shift, however, will be of value.
Revisiting Death: Implicit Bias and the Case of Jahi McMath
First published: 25 December 2018
Abstract
For nearly five years, bioethicists and neurologists debated whether Jahi McMath, an African American teenager, was alive or dead. While Jahi’s condition provides a compelling study for analyzing brain death, circumscribing her life status to a question of brain death fails to acknowledge and respond to a chronic, if uncomfortable, bioethics problem in American health care—namely, racial bias and unequal treatment, both real and perceived. Bioethicists should examine the underlying, arguably broader social implications of what Jahi’s medical treatment and experience represented. On any given day, disparities in the quality of health care and health outcomes for people of color in comparison to whites are evidenced in American hospitals and clinics. These disparities are not entirely explained by differences in patient education, insurance status, employment, income, expressed preference for treatments, and severity of disease. Instead, research indicates that, even for African Americans able to gain access to health care services and navigate institutional nuances, disparities persist across a broad range of services, including diagnostic screening and general medical care, mental health diagnosis and treatment, pain management, HIV-related care, and treatments for cancer, heart disease, diabetes, and kidney disease.
Why Bioethics Has a Race Problem
First published: 10 March 2016
Abstract
In the September-October 2001 issue of the Hastings Center Report, editor Gregory Kaebnick encouraged bioethicists to turn their attention toward “easily overlooked, relatively little-talked-about societal topics” such as race. In 2000 the president of the American Society for Bioethics had called for a more socially conscious bioethics. Race was risky territory, Kaebnick pointed out, but this challenge did not justify avoidance. Over the next fifteen years, the response to this editor’s invitation to examine the racial dimensions of medicine in the Report was limited both in quantity and in terms of the range of topics covered. All told, the bioethics community has not responded to the editor’s call for bioethicists to engage with the racial dimension of medicine, and the Report has not really come through on the tacit commitment made in 2001. The lack of interest in race matters evidenced in the Report as well as the American Journal of Bioethics has also prevailed in medical humanities journals, whose few pieces on race have tended to remove race relations from our current realities in two ways: some articles locate medical racism in the American past or in colonial Africa, while others analyze the medical disorders of fictional characters. Bioethicists have not embraced the opportunity to create a sociologically and historically informed bioethics that might be applied to the lives of black Americans and their unending health crisis.
Can Research on the Genetics of Intelligence Be “Socially Neutral”?
First published: 28 September 2015
Abstract
The history of research on the genetics of intelligence is fraught with social bias. During the eugenics era, the hereditary theory of intelligence justified policies that encouraged the proliferation of favored races and coercively stemmed procreation by disfavored ones. In the 1970s, Berkeley psychologist Arthur Jensen argued that black students’ innate cognitive inferiority limited the efficacy of federal education programs. The 1994 controversial bestseller The Bell Curve, by Richard J. Herrnstein and Charles Murray, rehashed the claim that race and class disparities stem from immutable differences in inherited intelligence, which could not be eliminated through social interventions. Today most scientists studying the genetics of intelligence distance themselves from this history of social bias by arguing that their research need not investigate intellectual differences between social groups. Rather, they argue, examining the heritability of intelligence can be socially neutral and may even help to reduce social inequities. I argue, however, that research on the genetics of intelligence cannot be socially neutral. Even if we divorce the heritability of intelligence from a eugenicist mission, measuring intelligence remains useful only as a gage of individuals’ appropriate positions in society. Research into the genetics of intelligence ultimately helps to determine individuals’ inherited capacity for particular social positions, even when researchers aim to modify the effects of inheritance.
Compassionate Imagining
First published: 04 March 2015
Abstract
I will always remember my first months at The Hastings Center as set against a backdrop of calls for social justice and the protection of vulnerable populations. Following weeks of civil unrest sparked by police brutality in Ferguson, Missouri, the fatal strangulation of Eric Garner, a black man, by a white New York police officer gave rise to “die-ins” across the country. I blogged for Bioethics Forum on the Ebola outbreaks in Guinea, Liberia, and Sierra Leone, with a focus on retrofitting governance systems that ignored a dangerous lack of health infrastructure and created populations vulnerable to public health emergencies. Back home in Virginia, I celebrated with family and friends the legalization of same-sex marriage after the Supreme Court let stand rulings in favor of it in five states. Voices of protest have focused our attention on the injustices faced by populations made vulnerable, particularly people of color, the poor, victims of public health crises, and lesbian, gay, bisexual, transgender, and queer communities.
Fevered Decisions: Race, Ethics, and Clinical Vulnerability in the Malarial Treatment of Neurosyphilis, 1922–1953
First published: 18 January 2015
Abstract
Syphilis occupies a unique position in the history of U.S. medicine and medical ethics. Given its widespread prevalence and variable presentation, syphilis was a major professional concern among late nineteenth- and early twentieth-century physicians. Syphilis was also at the center of perhaps the most famous example of medical racism in our history, the U.S. Public Health Service Syphilis Study at Tuskegee, in which officials followed the natural history of the disease in a cohort of black men for forty years without offering treatment, even once penicillin became available. In this essay, I call attention to a less well-known aspect of syphilis and its history. I examine one of the disease’s most dreaded manifestations, neurosyphilis (also known as general paresis or general paralysis of the insane), and its treatment via malarial inoculation from the 1920s into the 1950s. The goal of this treatment, dramatic even to observers at the time, was to produce spiking fevers that would kill the syphilitic spirochete and arrest the disease process. My focus will be on developments at St. Elizabeths Hospital, a large-scale federal psychiatric facility in the District of Columbia that served the city’s residents and members of the U.S. military. Physicians at St. Elizabeths were the first in the United States to experiment with malarial fever therapy, treating their initial cohort of patients in December of 1922.
Malarial fever therapy raised a host of ethical questions, rendered all the more complex from today’s vantage point by efforts to understand them within the context of the time. What sorts of risks, both from malaria and via indirect exposure, might be deemed acceptable in the treatment of a devastating and almost invariably fatal disease? How ought researchers and clinicians to have approached the question of consent, itself an evolving concept in the early decades of the twentieth century, when the disease they were targeting impaired a patient’s ability to reason effectively? Finally, at a time when segregated and inferior care for black Americans was the norm and when the black community bore a disproportionate burden of disease, who would have had access to malarial fever therapy, and at what cost?
The Risks of Race in Addressing Health Disparities
First published: July 2005
Abstract
There are undeniable differences among population groups in the incidence, prevalence, mortality, and social burden of serious diseases. However, some ways of representing the problem of health disparities may have unintended and unfortunate consequences. In particular, how we think about “race” and “ethnicity” carries grave risks.
Science and medical researchers often accept racial and ethnic categories as demographic truth, and they rarely parse the various ways these concepts are understood either in everyday speech or in scientific contexts. The medical scientific literature posits “race” and “ethnicity” as causal factors in a range of population differences: in access to health services, in the different effects of a given drug, in the presence of risk factors like hypertension, in behavior (think of “race and diet”), and in genetic susceptibility to disease. And now a pharmaceutical product’s viability can be assessed on the basis of demographic considerations that really only reflect marketing strategies (as happened with BiDil), not scientific knowledge of “racial” differences in drug metabolism.
Special Issues
A Critical Moment in Bioethics: Reckoning with Anti‐Black Racism through Intergenerational Dialogue
Volume 52, Issue S1
Abstract
As a field concerned with ethical issues in health and health care, particularly how structures, policies, and practices unfairly advantage some and disadvantage others, bioethics has a moral obligation to address the long-standing challenges that racism has posed to the overall health and well-being of Black, Indigenous, and Latinx people and other people of color. Arguably, the premature death and disease disproportionately affecting Black Americans and the well-documented association of such death and illness with racism are issues that have not gained due attention in bioethics. This multiauthored report highlights the intergenerational work of mostly Black scholars and aims to create an agenda for bioethics that addresses anti-Black racism and the ways in which this form of racism threatens the actualization of justice in health and health care, not only for Black people and other minoritized groups but also for all people.
This special report contains five major sections representing different approaches to scholarship, including theoretical, empirical, and narrative forms. The first section features two target articles focused on anti-Black racism and health care settings, with each article accompanied by two commentaries. The second section includes four essays thematically centered around anti-Black racism and health equity research and practice. Section three features four essays that explore anti-Black racism and bioethics. The next section consists of four essays framing a braver, bolder, and broader bioethics. We conclude with a powerful tribute to the late Marian Gray Secundy, a bioethics luminary, friend, colleague, role model, and mentor, and a tie that binds together many bioethics scholars who prioritize social justice in their scholarship and praxis.
From Hastings Center Bioethics Timeline:
1954: Brown v. Board of Education, Topeka, Kansas
In this landmark decision of the U.S. Supreme Court, the Court ruled unanimously (9-0) that state laws upholding racial segregation in public schools were unconstitutional. Undoing the doctrine of “separate but equal” established by the Supreme Court in Plessy v. Ferguson (1896), the Justices ruled “separate educational facilities are inherently unequal,” and violated the Equal Protection Clause of the 14th Amendment to the U.S. Constitution. The decision helped spur the Civil Rights movement.
1963: Simkins v. Moses H. Cone Memorial Hospital
On November 1, 1963, the Fourth Circuit Court of Appeals in Simkins v. Moses H. Cone Memorial Hospital ruled the separate-but-equal clause of the Hill-Burton Act unconstitutional. Since the U.S. Supreme Court refused to hear the case on appeal, the decision stood. The decision only affected hospitals receiving Hill-Burton funds. A 1964 federal court decision, Eaton v. Grubbs,broadened the prohibitions against racial discrimination to include hospitals that did not receive such funds.
Simkins v. Moses H. Cone Memorial Hospital, 323 F.2d 959 (4th Cir. 1963)
1964: Medical Committee for Human Rights
A group of health professionals founds the Medical Committee for Human Rights, which provided medical care to individuals fighting for human rights during the Mississippi “Freedom Summer.”
1965: Civil Rights Act
President Lyndon Johnson signs the Civil Rights Act, legally ending discrimination in public places based on race, color, religion, sex, and national origin under any program or activity receiving federal financial assistance.
1966: American Medical Association Addresses Discrimination
The AMA House of Delegates adopts a resolution to give the Judicial Council the authority to expel constituent societies for race discrimination in membership policies. There is a reaffirmation of cooperation between the AMA and the National Medical Association (NMA) and the first mention by the AMA of seeking ways to increase the presence of African Americans in medicine. A provision allowing the AMA to expel any state society found guilty of discrimination passed in 1968.
1968: American Medical Association Addresses Discrimination
The AMA House of Delegates adopts a resolution to give the Judicial Council the authority to expel constituent societies for race discrimination in membership policies. There is a reaffirmation of cooperation between the AMA and the National Medical Association (NMA) and the first mention by the AMA of seeking ways to increase the presence of African Americans in Medicine.
1980: Publication of Stephen Jay Gould’s The Mismeasure of Man
Stephen Jay Gould’s book disproved earlier scientific racist studies. Gould also openly criticized psychological testing, such as IQ tests, and the ranking of intelligence.
S. J. Gould, The Mismeasure of Man(New York: W. W. Norton, 1980). https://wwnorton.com/books/The-Mismeasure-of-Man/
1985: Heckler Report
Report of the Secretary’s Task Force on Black and Minority Health resulted in the creation of the Office of Minority Health in the Office of Health and Human Services.
2003: Publication of Brian Smedley, Adrienne Stith, and Alan Nelson’s Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care
Produced by the U.S. Institute of Medicine Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care.
B. Smedley, A. Stith, and A. Nelson, Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care (Washington, DC: National Academies Press, 2003). https://pubmed.ncbi.nlm.nih.gov/25032386/
2006: Publication of Sudhir Anand, Fabienne Peter, and Amartya Sen’s Public Health, Ethics, and Equity
This edited volume recognizes the importance of equity in public health ethics. It provides an interdisciplinary understanding of health equity and promotes the recognition of ethical issues in public health. It includes contributions from philosophers, anthropologists, economists, and public-health specialists on five major themes: defining health equity, health equity and social justice, responsibilities for health, and ethical issues in health evaluation.
S. Anand, F. Peter, and A. Sen, Public Health, Ethics, and Equity(Oxford: Oxford University Press, 2006). https://global.oup.com/academic/product/public-health-ethics-and-equity-9780199276370?cc=us&lang=en&
2006: Publication of Madison Powers and Ruth Faden’s Social Justice: The Moral Foundations of Public Health and Health Policy
In their book, Powers and Faden bring our attention to the principle of justice in securing public health and designing health policy. They point out the nondistributional aspects of justice.
M. Powers and R. Faden, Social Justice: The Moral Foundations of Public Health and Health Policy(New York: Oxford University Press, 2006). https://global.oup.com/academic/product/social-justice-9780195375138?cc=us&lang=en&
2009: AMA Apology to Discrimination against African American Physicians
The American Medical Association apologizes for its history of discrimination against African American physicians on July 28, 2008. It apologized for excluding black physicians from membership in the AMA, for listing black doctors as “colored” in its physician directory, and for failing to speak against federal funding of segregated hospitals and in favor of civil rights legislation.
https://www.ama-assn.org/about/ama-history/history-african-americans-and-organized-medicine
R. B. Baker et al., “African American Physicians and Organized Medicine, 1846-1968: Origins of a Racial Divide,” Journal of the American Medical Association 300, no. 3 (2008): 306-13.
https://jamanetwork.com/journals/jama/fullarticle/182255
2011: Body and Soul
Sociologist Alondra Nelson publishes Body and Soul which reports on African American responses to medical discrimination in the United States and focuses on health activism by the Black Panther Party.
A. Nelson, Body and Soul (Minneapolis: University of Minnesota Press, 2011).
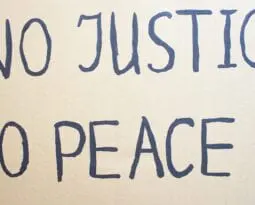
2020: Black Lives Matter Movement (George Floyd protests)
Created in 2013 in response to the death of Trayvon Martin and subsequent acquittal of his killer, the Black Lives Matter movement in 2020 becomes a massive “international response to state-sanctioned violence and anti-Black racism,” galvanizing around the videotaped, brutal killing of an unarmed black man named George Floyd by police officers in Minneapolis. Protests over police killings sweep many U.S. cities and the focus quickly expands to encompass racial injustice (and anti-Black racism in particular) in health care and other areas where the legacy of “scientific racism” perpetuates white privilege and structural discrimination again Black and brown people.
https://blacklivesmatter.com/about/
2020: American Academy of Pediatrics Apologizes for Its Racist Past
Joining the American Medical Association, where the AMA Institute for Ethics had carried out an investigation into racist membership policies prompting the organization to issue a public apology in 2008, the American Academy of Pediatrics in 2020 concluded an investigation into its prior racist membership policies and issued an apology, seeking a “path to equity.”
https://pediatrics.aappublications.org/content/146/3/e2020019794