Bioethics Forum Essay
Pregnancy, Brain Death, and the Right to Choose: Lessons from the Adriana Smith Case
Brain death during pregnancy presents complex ethical and legal questions regarding whether––and under what circumstances–any fetal interests or rights take precedence over those of a pregnant person. Here, we discuss the case of Adriana Smith and what it reveals about exceptions to advance care plans and the broader implications of policies that limit the autonomy of persons who are pregnant.
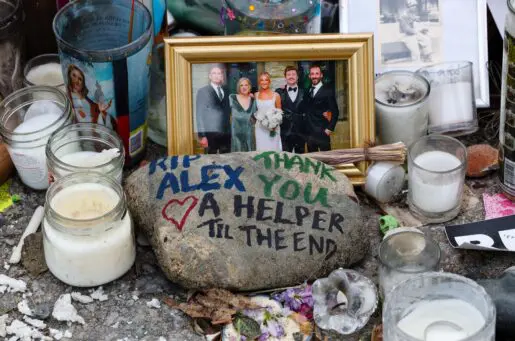
In February, physicians determined that Adriana Smith died by neurological criteria when she was nine weeks pregnant. Details about the circumstances that precipitated her death remain unclear, but the state of Georgia, where she lived and died, seems to require that she remain connected to machines that sustain her heartbeat and blood circulation until her baby can be delivered. Georgia is one of 31 states that restricts the discontinuation of life support for pregnant patients. Smith’s family has clarified that while they want to continue Adriana’s pregnancy, they believe the decision to do so “should have been left to [them]–not the state.”
State laws that restrict decision-making by patients (or their surrogates) may result in some people not having their values and preferences honored. Thus, it is critically important for bioethicists and clinicians to address the social, structural, and political forces that shape and give rise to ethical dilemmas in reproductive care.
It is worth considering whether Adriana Smith’s case might have been handled differently prior to the fall of Roe, and how evolving state abortion laws might override maternal advance directives or otherwise alter end-of-life care during pregnancy. Twenty-six states invalidate advance care plans for pregnant persons–but only nine jurisdictions disclose these exceptions in state advance directive documents. While the American College of Obstetricians and Gynecologists recommends that physicians respect the treatment preferences of all patients regardless of their pregnancy status, the case of Adriana Smith is not unique insofar as legal intrusions upon the rights of pregnant and postpartum people are common.
Notably, advance directive pregnancy restrictions existed before the Dobbs decision, but post-Dobbs efforts to establish fetal personhood have contributed to a rebalancing of fetal rights that correlates with diminished maternal decision-making authority. This, in turn, has led to its logical end of criminalizing maternal behavior. In the United States, pregnant patients have been arrested, forced to undergo cesarean sections, incarcerated following traumatic pregnancy losses, and otherwise deprived of the right to due process in the name of fetal protection. Restrictions in end-of-life decision making will likely lead to the same criminalization outcomes.
The burdens of pregnancy criminalization are disproportionately borne by Black women living in the U.S., who are not only three times more likely to die from preventable pregnancy complications than their white counterparts, but are also 10 times more likely to be reported to law enforcement or social services for matters related to their pregnancy and birth. As noted by legal scholar Kimberly Mutcherson, these inequities are exacerbated by laws that cannot capture the complexities of pregnancy or account for the vast variability of obstetric emergencies.
The criminalization of pregnancy–and the rebalancing of fetal rights relative to those afforded to others–demand the attention of bioethicists, who are perhaps uniquely positioned to analyze reproductive injustices wrought by the erosion of a pregnant person’s rights to refuse treatment. Pregnancy complications may require invoking advance care plans; bioethicists and clinicians arguably have a duty to articulate how pregnancy might alter whether and how a patient’s stated end-of-life preferences are applied.
Bioethicists must engage in public awareness and advocacy efforts to educate medical professionals and members of the public who might not know that the state can override the wishes and preferences of incapacitated people if they are pregnant. Fostering conversations about the limits of advance directives is a function of our duty to support the right of all patients to make fully informed and voluntary decisions–a principle at the very core of informed consent, respect for persons, and shared decision-making. Furthermore, clear and honest communication about highly publicized and complex cases like Adriana Smith’s is key to rebuilding public trust in science and health care.
Elsewhere, we have addressed how bioethicists ought to recognize, name, and transform the social and structural forces that combine to limit the agency, visibility, and voice of marginalized people, especially those who may become pregnant. As Dorothy Roberts, Michele Goodwin, Kimberly Mutcherson, and other intersectional bioethics and legal scholars have long argued, policies that restrict reproductive autonomy have historically burdened Black mothers first, then eventually expanded to limit the reproductive rights of all persons who can become pregnant. Many of us have called for broader and bolder bioethics frameworks to help bioethicists systematically and deliberately respond to long-standing health inequities, including the rise in maternal deaths among Black women. We have also argued that bioethicists and clinicians ought to support meaningful discourse on polarizing topics in reproductive ethics by clarifying ambiguous terms in order to move policy debates from matters of semantics to matters of substance.
The case of Adriana Smith highlights intersectional bioethics issues from the point of conception to end-of-life care while illuminating the often complex interplay between reproductive medicine and the law. Recent empirical work shows that bioethicists want to engage with social justice issues and that clear and honest communication with patients and the public strengthens institutional trustworthiness as it relates to equitable maternal health care. Where Smith is concerned, bioethicists can engage meaningfully by redirecting the debate about the specific decisions of her family or clinical team toward a broader conversation about the structures, policies, and practices that prevent pregnant patients and their surrogates from having the ability to make decisions about life-sustaining treatment.
This case raises complicated questions about how end-of-life decision-making authority and abortion bans can coexist in the post-Roe era–and whether they should. The right of all persons to have self-determination over their care at the end of life ought to be inviolable, regardless of their pregnancy status. Thus, Adriana Smith’s life and death must not be deployed as another political talking point, but rather as a sobering call to action for bioethicists and clinicians, who must collaborate to support incapacitated patients and their surrogates while advocating for policies that protect the autonomy and dignity of all people across their entire life course.
Any opinions, conclusions, and recommendations expressed in this essay are those of the authors and do not represent the views of Baylor College of Medicine, The Hastings Center for Bioethics, or UT Health Houston.
Sophie L. Schott, BA, GCert, is a second-year medical student in Houston, Texas, and a clinical research coordinator in the Center for Medical Ethics and Health Policy at Baylor College of Medicine. @MyBestSchott
Faith E. Fletcher, PhD, MA, is an associate professor in the Center for Medical Ethics and Health Policy at Baylor College of Medicine. She is also a Hastings Center Fellow and a Greenwall Bioethics Faculty Scholar. @FaithEFletcher
Claire I. Horner, JD, MA, HEC-C, is an associate professor in the Center for Medical Ethics and Health Policy at Baylor College of Medicine. She is also a clinical ethicist at Baylor St. Luke’s Medical Center.
Virginia A. Brown, PhD, MA, is a research scholar in health equity and population health at The Hastings Center for Bioethics. @VirginiaABrown












I agree entirely with this paper. I would go even further and establish some clear rules based on pregnancy duration and viabiliity. The added problem with maintaining the pregnancy, raises also issues of the health of a child maitained in this manner and concerns for is neurodevelopmental issues and the child’s entire lifetime… Would the child be resentful that she or he were maitained alive in this manner? There are multiple facets that this case raises in addition to those so well described by the authors.
Thank you all so very much for this well-crafted perspective and recommendation(s). …passing this along to my students and colleagues…
Thank you to the authors and the Hastings Center for addressing this case and the complex issues involved. This is truly an intersectional case of utmost importance in present day America. I worry about ethicists losing credibility if we become too partisan in what is a political culture war issue. However, I’m more concerned for our culture if we do not engage in these fraught issues. Thank you for threading the needle, as we continue to sew.
This is a tragic case but it’s an odd one to use to raise the issue of restrictive abortion laws because the Georgia AG publicly and specifically said that there is no legal requirement to keep this poor woman’s body on organ support (though he called it life support.) But if we want to raise important issues out of this case, one could reasonably ask: what do we mean by brain “death” if someone who is dead is capable of nurturing and bringing forth new life? If even the GOP AG in Georgia says the hospital has no obligation to keep her on the machines, then why does the hospital and family feel so uncomfortable removing them?
I would hardly call her “capable of nurturing and bringing forth new life” when she needs extensive medical intervention to do so.
I’ve read that the reason the hospital won’t remove the machines is because they’re worried about the state coming after them for killing the potentially non-viable fetus, as it will very likely die once life support has been pulled. Her family wants her to be removed from life support but they also know the situation the hospital is in with regards to the states abortion ban and concerns about being held legally accountable for the death of that fetus. It is why her family is even speaking out in the first place about her being used an incubator for this fetus who might not live once removed from the mother, because they don’t want to see their daughters body used this way.
Thank you for sharing this and shining light on such a complex and heartbreaking case. The story of Adriana Smith, a woman declared brain dead by neurological criteria at nine weeks pregnant in Georgia, is really baffling. It shows how deeply connected reproductive rights, bioethics, and end of life care have become, especially in the post- Roe era. The idea that the state could require her to remain on life support until the baby is viable shows just how far the law can go to prioritize fetal interest over a pregnant persons, and their families, autonomy.
What struck me the most is the fact that the state could make the decision to continue life support regardless of the families wishes. Georgia is one of 31 states that restrict the discontinuation of life support for pregnant patients. It makes me wonder if there are any other medical situations where the state can intervene and say, “no, this patient cannot have care withdrawn”. While Adriana’s family did wish to continue life support, that does not make the experience any easier for them or lessen the emotional weight of their grief.
The state’s mandate to keep Adriana on life support to continue to grow the 9 week fetus essentially forces the deceased person to function as a human incubator, or a vessel for gestation. Although organ donation is not the same, I can’t help but draw the comparison. When a patient who is not pregnant is declared brain dead, organ donation decisions are made based on prior consent or next of kin, which honors the individual’s autonomy and dignity. The state does not have a say in that process. Typically, life support may be continued for a day or two but not for sixteen weeks – as seen in Adriana’s case.
As a healthcare worker, it is extremely difficult mentally, emotionally, and ethically to provide futile care. This case is a reminder of how connected law and medicine can be and how it can strip away humanity from patients and families.
Dear Authors,
As a Black American woman and soon-to-be psychiatric nurse practitioner, I was deeply moved by your article, “Pregnancy, Brain Death, and the Right to Choose: Lessons from the Adriana Smith Case.” Your thoughtful analysis of the legal and ethical forces shaping end-of-life care during pregnancy resonated powerfully with both my lived experience and my professional aspirations.
I was especially struck by your clear depiction of how Georgia’s Living Infants Fairness and Equality (LIFE) Act treated Adriana Smith—not as a patient with rights and values but as a vessel whose autonomy was legally erased once her fetus had a detectable fetal heartbeat (usually at six weeks). Your article highlighted a disturbing reality: the state of Georgia assumed decision-making power for Ms. Smith and revoked the authority that should have remained with her family, turning a profoundly personal tragedy into a rigid legal mandate. Ms. Smith was a 30-year-old nurse, mother, and daughter—beloved by her family, who should have been trusted to make compassionate and informed decisions in her best interest. Her story reminds us that if bodily autonomy can be taken from someone after death, then bodily autonomy is certainly at risk for all of us in life.
Your examination of the widespread—and often hidden—restrictions on advance directives for pregnant individuals is critically important. I was alarmed to learn that twenty-six states invalidate advance directives during pregnancy, with only a minority (9) even disclosing these limitations.
What resonated most with me was your acknowledgment that these intrusions on personal autonomy do not affect everyone equally. Black women in the United States already face the highest maternal mortality rates and are disproportionately criminalized during pregnancy. As you noted, policies created under the guise of protecting fetal personhood frequently become mechanisms for policing and punishing the bodies and decisions of marginalized women first. The post-Dobbs expansion of fetal personhood has undoubtedly made an already dangerous situation even more fraught for those most vulnerable.
As a Black female attorney and future psychiatric nurse practitioner, I am acutely aware of the consequences—both legally and in practice—of denying the personal autonomy of pregnant individuals, criminalizing pregnancy in favor of fetal rights, and prohibiting incapacitated pregnant patients and their surrogates from making decisions about medical care and end-of-life wishes. There is no doubt that these policies will further deepen generational fear and mistrust of the medical profession within the Black community.
Your article powerfully calls on bioethicists and clinicians to advocate for change. If we fail to do so, pregnant people within marginalized communities will once again hide in the shadows, where they either self-treat or seek care from unqualified individuals, risking grave harm and irreparable consequences. I share your conviction that silence makes us complicit in systems that strip patients of agency at their most vulnerable moments. The right to make decisions about one’s own body should never be negotiable, and pregnancy must never transform a person from a rights-holder into a legal exception.
I aspire to work in a healthcare landscape where every patient, pregnant or not, can rely on their documented wishes—and the decisions of their designated surrogates—being honored and respected. Thank you for sharing Adriana Smith’s story with such clarity and for challenging current and future healthcare professionals, like myself, to safeguard the dignity and autonomy of all people capable of pregnancy.