Bioethics Forum Essay
Honoring Alex Pretti’s Moral Courage and the Cost of Caring
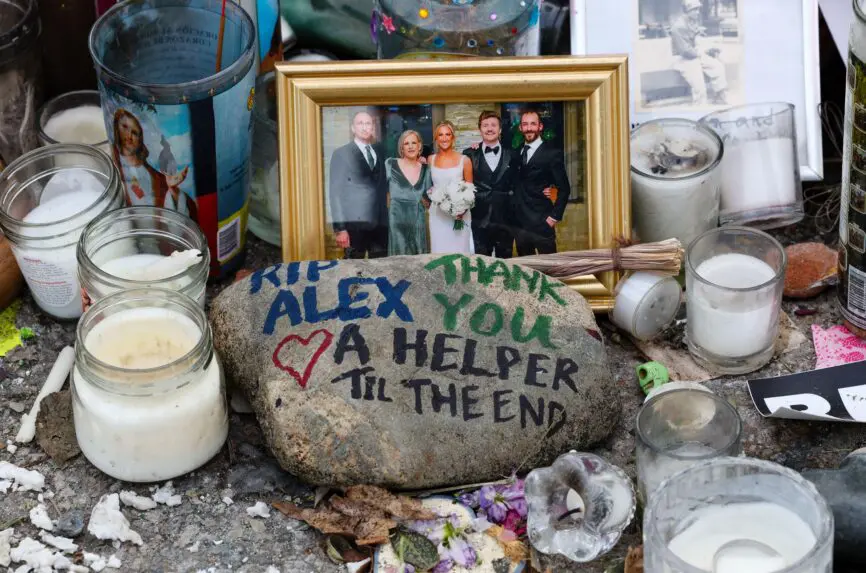
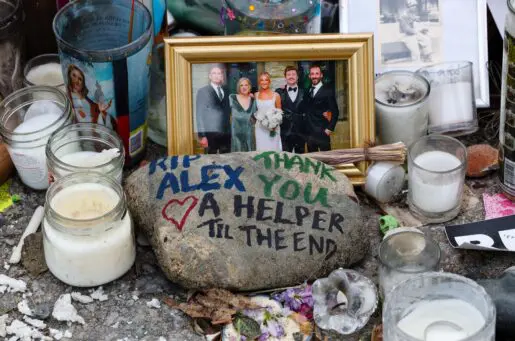
The death of Alex Pretti, an ICU nurse who was killed last month in an anti-immigration protest in Minneapolis, is, first and foremost, a devastating loss for his loved ones. But it has also shaken the nursing profession to the core.
People often encounter nurses at the bedside when they are ill or someone close to them is ill. But nurses also have a long history of advocating for social justice in their communities, speaking out against unjust policies, challenging unsafe practices, and advancing public health reforms.
The 2025 Code of Ethics for Nurses reflects this activism. It calls on all nurses to be civically engaged and to work toward policies and systems that have positive ends for the communities in which we live and work. Alex met this call.
Alex used his ICU training to help someone in need; it was second nature to him and reflected his primary obligation as a registered nurse to protect the rights and well-being of patients, families, and communities. He lost his life because he helped a woman during a protest against federal immigration action in Minneapolis. Pretti stepped in front of the woman, who was on the ground, to protect her from being pepper sprayed by U.S. Border Patrol agents. Agents then pinned Pretti to the ground and shot him.
Nurses are no strangers to conflict and moral turmoil. They take a professional and ethical oath to care for anyone — victim or perpetrator — regardless of their identity or ideological belief. But Alex’s death exposes a stark and troubling reality for every nurse and healthcare provider: Immigration enforcement agents are now occupying spaces that should be protected in hospitals, waiting rooms, lobbies, and clinics. These are places where patients must feel safe and trust that they will receive care without discrimination and be protected from intimidation.
The presence of immigration enforcement agents in these places is creating profound moral distress and a climate of deep fear for all those who deliver care and for the people who need it most within these buildings. Nurses and other healthcare providers are caught in the age-old dilemma between what is ethical and what is legal: They question what they ought to do when faced with immigration enforcement agents standing outside hospital rooms and observing the care they are ethically and professionally obligated to protect.
When nurses and other healthcare providers cannot meet their ethical duties to protect the rights and welfare of their patients, this distress can intensify into a deeper wound with lingering residue of regret and a searing violation of their sense of integrity.
For their part, patients may withhold critical health information, become afraid to ask questions, and mistrust health professionals when immigration enforcement agents are present. Patients who are immigrants are most vulnerable to these harms, but other patients may also experience them. The harms – to healthcare providers and patients – can ultimately compromise ethical decision-making, patient-and family-centered care, and the overall quality of care that all patients deserve, and healthcare providers are trained to deliver.
The patients and families cared for by Alex will always remember him. Nurses will remember Alex’s sacrifice – that his caring extended beyond the walls of his hospital to the stranger he protected in his community.
Nurses can honor Alex’s moral courage through our individual and professional resolve. We must say no more to the infiltration of immigration enforcement into healthcare spaces that were previously off limits to them. We must speak out on re-establishing “safe zones,” hospital-wide policies that limit enforcement access, and confidential reporting mechanisms that reflect the humanity of the nursing profession towards those we took an oath to serve.
May a better and more humane world prevail, reminding each of us that moral courage carries risk, but it also helps us rise to the occasion when change and moral repair are needed most. We are at that moment.
Connie M. Ulrich, PhD, RN, is a registered nurse and professor of nursing and of medical ethics and health policy at the University of Pennsylvania School of Nursing and a Hastings Center Fellow. LinkedIn: connieulrich1, X: @cm_ulrich
Mary D. Naylor, PhD, RN, is a registered nurse and professor of gerontology and nursing at Penn’s School of Nursing. LinkedIn: Mary_Naylor, X: @MaryDNaylor
Martha A.Q. Curley, PhD, RN, is a registered nurse and professor of pediatric nursing at Penn’s School of Nursing. LinkedIn: Martha-a-q-curley, X: maqcurley, Bluesky: @maqc.bsky.social











Thank you for this and I agree with all of your recommendations. I also wonder about the health care professionals (HCPs) employed in the so-called “detention facilities”. There must be some serious ethical concerns about the practices of such HCPs, similar to those that work(ed) in concentration camps or in Israeli prisons. I hear absolutely nothing about what is going on for them… I could imagine that at least some of them choose to accept such employment as a matter of harm reduction but are witness to horrid conditions. Based on reporting these HCPs either participate in or witness the refusal of medical care to people who desperately need it. I’ve read reports about people who are “detained” (abducted) and do not have access to their asthma inhaler or essential medications… what role are health care providers playing in all of this? Is there guidance for them based on these other situations that could be applied here? Is the right ethical statement “do not take employment as a health care provider in an ICE facility because it is unethical” or do we have guidance for them to do so to reduce harm? What kind of regulations are in place to ensure health care access in ICE facilities?
I know that in Washington state there is currently legislation being considered:
SSB 6286 – Fines for Private Detention Facilities That Block DOH Inspections Last session, HB 1232 gave the Department of Health authority to inspect private detention facilities but DOH has since been denied entry. This bill creates civil fines for facilities that refuse to permit inspections. The bill received a do-pass from Senate Human Services and is scheduled for a public hearing in the Senate Ways and Means Committee on February 19.
We should also promote legislation like this.
Thank you for this publication on Alex Pretti and the ethics of care in nursing. I remember family discussion the horrors of Senator McCarthy decades ago . How horrible and frightening it was for my family thinking the U.S. had become unsafe for those in the public eye and for “ordinary people”. Then came Khruschev and his warnings, “”We will bury you” and replies of “Better Dead than Red”. Take-cover drills where we crawled under our desks to prepare for when a bomb might come. The Cuban Missle Crisis with threats of missles aimed at my preciousManhattan and the World Trade Towers attacked and destroyed coinciding with the U.S. heroes who lost their lives having made a choice to take down the plane they were on rather than let it crash into our government structures. Each horror was considered the worst we would see in the United States of America. The state of our country today is something I never would have expected to have come to fruition, and yet…here we are. Alex Pretti lost his life protecting someone from harm. Yet, this time, the harm comes from within our own citizens. It is a horror I never would have anticipated, brought about by the casting of votes for unbridled power. For Alex Pretti.’s memory, and for all of you practicing your professions, finding ways to follow our codes of ethics, I thank youfor your determination and courage to care.